Page 64 - Read Online
P. 64
Sawada et al. Mini-invasive Surg 2021;5:6 I http://dx.doi.org/10.20517/2574-1225.2020.100 Page 7 of 11
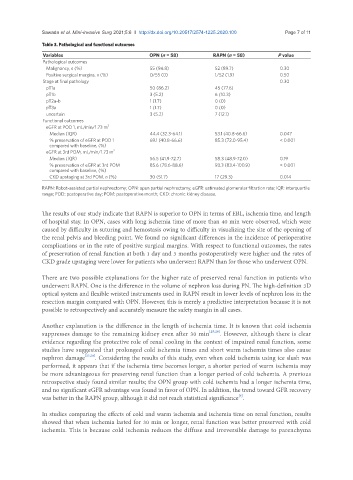
Table 3. Pathological and functional outcomes
Variables OPN (n = 58) RAPN (n = 58) P value
Pathological outcomes
Malignancy, n (%) 55 (94.8) 52 (89.7) 0.30
Positive surgical margins, n (%) 0/55 (0) 1/52 (1.9) 0.50
Stage at final pathology 0.30
pT1a 50 (86.2) 45 (77.6)
pT1b 3 (5.2) 6 (10.3)
pT2a-b 1 (1.7) 0 (0)
pT3a 1 (1.7) 0 (0)
uncertain 3 (5.2) 7 (12.1)
Functional outcomes
eGFR at POD 1, mL/min/1.73 m 2
Median (IQR) 44.4 (32.3-64.1) 53.1 (40.8-66.6) 0.047
% preservation of eGFR at POD 1 69.1 (40.8-66.6) 85.3 (72.0-95.4) < 0.001
compared with baseline, (%)
eGFR at 3rd POM, mL/min/1.73 m 2
Median (IQR) 56.5 (41.9-72.7) 58.3 (48.9-72.0) 0.19
% preservation of eGFR at 3rd POM 85.6 (78.6-88.6) 93.3 (83.4-100.9) < 0.001
compared with baseline, (%)
CKD upstaging at 3rd POM, n (%) 30 (51.7) 17 (29.3) 0.014
RAPN: Robot-assisted partial nephrectomy; OPN: open partial nephrectomy; eGFR: estimated glomerular filtration rate; IQR: interquartile
range; POD: postoperative day; POM: postoperative month; CKD: chronic kidney disease.
The results of our study indicate that RAPN is superior to OPN in terms of EBL, ischemia time, and length
of hospital stay. In OPN, cases with long ischemia time of more than 40 min were observed, which were
caused by difficulty in suturing and hemostasis owing to difficulty in visualizing the site of the opening of
the renal pelvis and bleeding point. We found no significant differences in the incidence of perioperative
complications or in the rate of positive surgical margins. With respect to functional outcomes, the rates
of preservation of renal function at both 1 day and 3 months postoperatively were higher and the rates of
CKD grade upstaging were lower for patients who underwent RAPN than for those who underwent OPN.
There are two possible explanations for the higher rate of preserved renal function in patients who
underwent RAPN. One is the difference in the volume of nephron loss during PN. The high-definition 3D
optical system and flexible wristed instruments used in RAPN result in lower levels of nephron loss in the
resection margin compared with OPN. However, this is merely a predictive interpretation because it is not
possible to retrospectively and accurately measure the safety margin in all cases.
Another explanation is the difference in the length of ischemia time. It is known that cold ischemia
suppresses damage to the remaining kidney even after 30 min [25,26] . However, although there is clear
evidence regarding the protective role of renal cooling in the context of impaired renal function, some
studies have suggested that prolonged cold ischemia times and short warm ischemia times also cause
nephron damage [27,28] . Considering the results of this study, even when cold ischemia using ice slush was
performed, it appears that if the ischemia time becomes longer, a shorter period of warm ischemia may
be more advantageous for preserving renal function than a longer period of cold ischemia. A previous
retrospective study found similar results; the OPN group with cold ischemia had a longer ischemia time,
and no significant eGFR advantage was found in favor of OPN. In addition, the trend toward GFR recovery
was better in the RAPN group, although it did not reach statistical significance .
[6]
In studies comparing the effects of cold and warm ischemia and ischemia time on renal function, results
showed that when ischemia lasted for 30 min or longer, renal function was better preserved with cold
ischemia. This is because cold ischemia reduces the diffuse and irreversible damage to parenchyma