Page 444 - Read Online
P. 444
Page 8 of 14 Choi et al. Mini-invasive Surg 2021;5:43 https://dx.doi.org/10.20517/2574-1225.2021.73
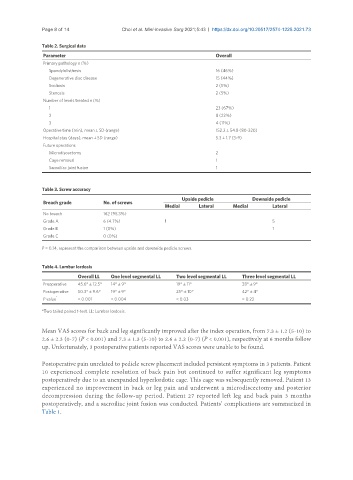
Table 2. Surgical data
Parameter Overall
Primary pathology n (%)
Spondylolisthesis 16 (46%)
Degenerative disc disease 15 (44%)
Scoliosis 2 (5%)
Stenosis 2 (5%)
Number of levels treated n (%)
1 23 (67%)
2 8 (22%)
3 4 (11%)
Operative time (min), mean ± SD (range) 152.2 ± 54.8 (80-320)
Hospital stay (days), mean ± SD (range) 5.3 ± 1.7 (3-9)
Future operations
Microdiscectomy 2
Cage removal 1
Sacroiliac joint fusion 1
Table 3. Screw accuracy
Upside pedicle Downside pedicle
Breach grade No. of screws
Medial Lateral Medial Lateral
No breach 162 (95.3%)
Grade A 6 (4.7%) 1 5
Grade B 1 (0%) 1
Grade C 0 (0%)
P = 0.14, represent the comparison between upside and downside pedicle screws.
Table 4. Lumbar lordosis
Overall LL One level segmental LL Two level segmental LL Three level segmental LL
Preoperative 45.6° ± 12.5° 14° ± 9° 19° ± 11° 38° ± 9°
Postoperative 50.3° ± 9.6° 19° ± 9° 25° ± 10° 42° ± 4°
P value * < 0.001 < 0.004 < 0.03 = 0.23
*Two tailed paired t-test. LL: Lumbar lordosis.
Mean VAS scores for back and leg significantly improved after the index operation, from 7.3 ± 1.2 (5-10) to
2.6 ± 2.3 (0-7) (P < 0.001) and 7.3 ± 1.3 (5-10) to 2.6 ± 2.2 (0-7) (P < 0.001), respectively at 6 months follow
up. Unfortunately, 3 postoperative patients reported VAS scores were unable to be found.
Postoperative pain unrelated to pedicle screw placement included persistent symptoms in 3 patients. Patient
10 experienced complete resolution of back pain but continued to suffer significant leg symptoms
postoperatively due to an unexpanded hyperlordotic cage. This cage was subsequently removed. Patient 13
experienced no improvement in back or leg pain and underwent a microdiscectomy and posterior
decompression during the follow-up period. Patient 27 reported left leg and back pain 3 months
postoperatively, and a sacroiliac joint fusion was conducted. Patients’ complications are summarized in
Table 1.