Page 442 - Read Online
P. 442
Choi et al. Mini-invasive Surg 2021;5:43 https://dx.doi.org/10.20517/2574-1225.2021.73 Page 7 of 14
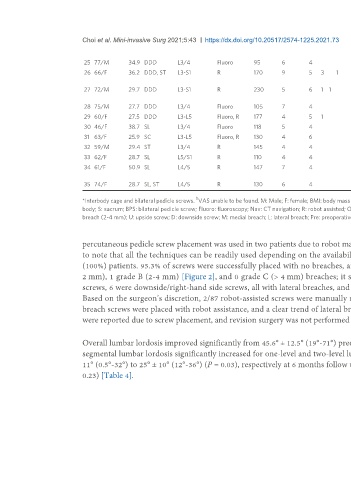
25 77/M 34.9 DDD L3/4 Fluoro 95 6 4 63 63 12 20 10/10 1/1 Transient neuralgia
26 66/F 36.2 DDD, ST L3-S1 R 170 9 5 3 1 2 42 44 40 41 8/8 7/7 Postoperative fall, recurrent
symptoms, plan for reoperation
27 72/M 29.7 DDD L3-S1 R 230 5 6 1 1 2 59 55 50 48 6/6 2/2 Persistent left leg/back pain,
SIJ fusion
28 75/M 27.7 DDD L3/4 Fluoro 105 7 4 53 59 12 16 8/8 1/0 Urosepsis, delirium
29 60/F 27.5 DDD L3-L5 Fluoro, R 177 4 5 1 1 19 33 0.75 12 5/5 0/1
30 46/F 38.7 SL L3/4 Fluoro 118 5 4 54 54 10 10 8/- 2/- Wound infection
31 63/F 25.9 SC L3-L5 Fluoro, R 130 4 6 57 57 19 28 8/8 0/4
b
32 59/M 29.4 ST L3/4 R 145 4 4 38 46 7 9 8/8
33 62/F 28.7 SL L5/S1 R 110 4 4 71 57 35 22 8/8 0/0
34 61/F 50.9 SL L4/5 R 147 7 4 51 24 51 26 9/9 7/7 Respiratory distress, prolonged
ICU stay
35 74/F 28.7 SL, ST L4/5 R 130 6 4 49 56 10 16 7/7 5/5
b
*Interbody cage and bilateral pedicle screws. VAS unable to be found. M: Male; F: female; BMI: body mass index; SL: spondylolisthesis; DDD: degenerative disc disease; ST: stenosis; SC: scoliosis; L: lumbar vertebral
body; S: sacrum; BPS: bilateral pedicle screw; Fluoro: fluoroscopy; Nav: CT navigation; R: robot assisted; OR: operating room; LOS: length of stay; NB: no breach; A: Spitz grade A breach (< 2 mm); B: Spitz grade B
breach (2-4 mm); U: upside screw; D: downside screw; M: medial breach; L: lateral breach; Pre: preoperative; F/U: follow-up; Postop: postoperative.
percutaneous pedicle screw placement was used in two patients due to robot malfunction and in the other cases due to the surgeon’s preference. It is important
to note that all the techniques can be readily used depending on the availability of the equipment. Six months follow-up CT scans were obtained from 35
(100%) patients. 95.3% of screws were successfully placed with no breaches, and 7 total screw breaches were identified (4.7%); 6 were graded A breaches (<
2 mm), 1 grade B (2-4 mm) [Figure 2], and 0 grade C (> 4 mm) breaches; it showed no statistically significant difference with P = 0.14. Of the 7 breached
screws, 6 were downside/right-hand side screws, all with lateral breaches, and a medial breach was observed for the 1 upside/left-hand side screw [Table 3].
Based on the surgeon’s discretion, 2/87 robot-assisted screws were manually repositioned, both of which were later identified as breaches. In our series, all
breach screws were placed with robot assistance, and a clear trend of lateral breach laterality is seen in the downside screws. In our cohort, no complications
were reported due to screw placement, and revision surgery was not performed due to screw malposition.
Overall lumbar lordosis improved significantly from 45.6° ± 12.5° (19°-71°) preoperatively to 50.3° ± 9.6° (25°-67°) at 6 months follow up (P < 0.001). Similarly,
segmental lumbar lordosis significantly increased for one-level and two-level lumbar fusions, from 14° ± 9° (-8°-35°) to 19° ± 9° (2°-36°) (P < 0.004) and 19° ±
11° (0.5°-32°) to 25° ± 10° (12°-36°) (P = 0.03), respectively at 6 months follow up. For three-level fusions, segmental lordosis did not significantly change (P =
0.23) [Table 4].