Page 157 - Read Online
P. 157
Page 4 of 8 Toma et al. Mini-invasive Surg 2018;2:21 I http://dx.doi.org/10.20517/2574-1225.2018.24
A B
Figure 2. Representative images of NADENs from case 3. (A) Endoscopic image, arrow: NADENs, arrowhead: Brunner gland; (B) upper GI
series images, arrow: NADENs
A B
C D
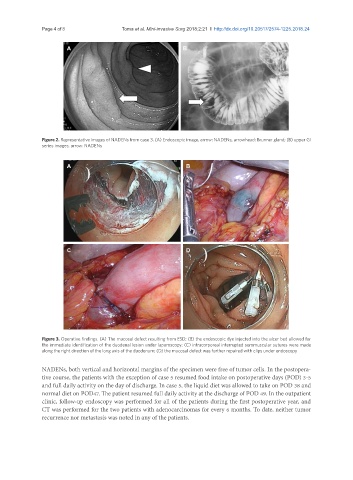
Figure 3. Operative findings. (A) The mucosal defect resulting from ESD; (B) the endoscopic dye injected into the ulcer bed allowed for
the immediate identification of the duodenal lesion under laparoscopy; (C) intracorporeal interrupted seromuscular sutures were made
along the right direction of the long axis of the duodenum; (D) the mucosal defect was further repaired with clips under endoscopy
NADENs, both vertical and horizontal margins of the specimen were free of tumor cells. In the postopera-
tive course, the patients with the exception of case 5 resumed food intake on postoperative days (POD) 3-5
and full daily activity on the day of discharge. In case 5, the liquid diet was allowed to take on POD 38 and
normal diet on POD47. The patient resumed full daily activity at the discharge of POD 49. In the outpatient
clinic, follow-up endoscopy was performed for all of the patients during the first postoperative year, and
CT was performed for the two patients with adenocarcinomas for every 6 months. To date, neither tumor
recurrence nor metastasis was noted in any of the patients.