Page 10 - Read Online
P. 10
Page 4 of 11 Kikuchi et al. Mini-invasive Surg 2024;8:8 https://dx.doi.org/10.20517/2574-1225.2023.88
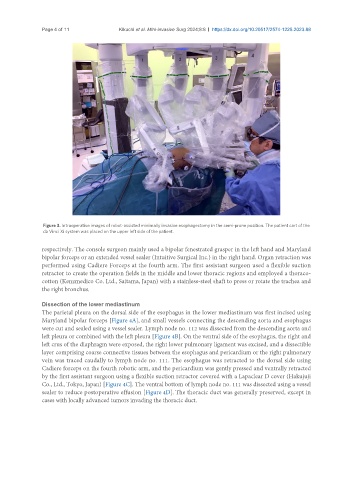
Figure 3. Intraoperative images of robot-assisted minimally invasive esophagectomy in the semi-prone position. The patient cart of the
da Vinci Xi system was placed on the upper left side of the patient.
respectively. The console surgeon mainly used a bipolar fenestrated grasper in the left hand and Maryland
bipolar forceps or an extended vessel sealer (Intuitive Surgical Inc.) in the right hand. Organ retraction was
performed using Cadiere Forceps at the fourth arm. The first assistant surgeon used a flexible suction
retractor to create the operation fields in the middle and lower thoracic regions and employed a thoraco-
cotton (Kenzmedico Co. Ltd., Saitama, Japan) with a stainless-steel shaft to press or rotate the trachea and
the right bronchus.
Dissection of the lower mediastinum
The parietal pleura on the dorsal side of the esophagus in the lower mediastinum was first incised using
Maryland bipolar forceps [Figure 4A], and small vessels connecting the descending aorta and esophagus
were cut and sealed using a vessel sealer. Lymph node no. 112 was dissected from the descending aorta and
left pleura or combined with the left pleura [Figure 4B]. On the ventral side of the esophagus, the right and
left crus of the diaphragm were exposed, the right lower pulmonary ligament was excised, and a dissectible
layer comprising coarse connective tissues between the esophagus and pericardium or the right pulmonary
vein was traced caudally to lymph node no. 111. The esophagus was retracted to the dorsal side using
Cadiere forceps on the fourth robotic arm, and the pericardium was gently pressed and ventrally retracted
by the first assistant surgeon using a flexible suction retractor covered with a Lapaclear D cover (Hakujuji
Co., Ltd., Tokyo, Japan) [Figure 4C]. The ventral bottom of lymph node no. 111 was dissected using a vessel
sealer to reduce postoperative effusion [Figure 4D]. The thoracic duct was generally preserved, except in
cases with locally advanced tumors invading the thoracic duct.