Page 79 - Read Online
P. 79
Page 8 of 16 Annibali et al. Mini-invasive Surg 2022;6:12 https://dx.doi.org/10.20517/2574-1225.2021.101
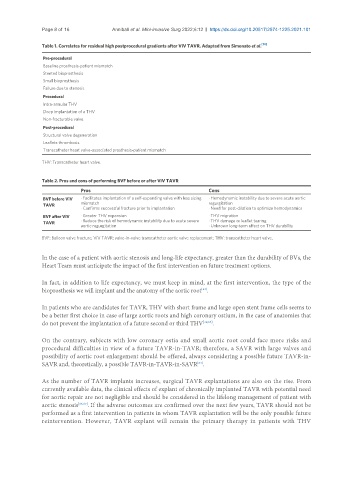
Table 1. Correlates for residual high postprocedural gradients after ViV TAVR. Adapted from Simonato et al. [14]
Pre-procedural
Baseline prosthesis-patient mismatch
Stented bioprosthesis
Small bioprosthesis
Failure due to stenosis
Procedural
Intra-annular THV
Deep implantation of a THV
Non-fracturable valve
Post-procedural
Structural valve degeneration
Leaflets thrombosis
Transcatheter heart valve-associated prosthesis-patient mismatch
THV: Transcatheter heart valve.
Table 2. Pros and cons of performing BVF before or after ViV TAVR
Pros Cons
BVF before ViV · Facilitates implantation of a self-expanding valve with less sizing · Hemodynamic instability due to severe acute aortic
TAVR mismatch regurgitation
· Confirms successful fracture prior to implantation · Need for post-dilation to optimize hemodynamics
BVF after ViV · Greater THV expansion · THV migration
TAVR · Reduce the risk of hemodynamic instability due to acute severe · THV damage or leaflet tearing
aortic regurgitation · Unknown long-term effect on THV durability
BVF: Balloon valve fracture; ViV TAVR: valve-in-valve transcatheter aortic valve replacement; THV: transcatheter heart valve.
In the case of a patient with aortic stenosis and long-life expectancy, greater than the durability of BVs, the
Heart Team must anticipate the impact of the first intervention on future treatment options.
In fact, in addition to life expectancy, we must keep in mind, at the first intervention, the type of the
bioprosthesis we will implant and the anatomy of the aortic root .
[64]
In patients who are candidates for TAVR, THV with short frame and large open stent frame cells seems to
be a better first choice in case of large aortic roots and high coronary ostium, in the case of anatomies that
do not prevent the implantation of a future second or third THV [39,65] .
On the contrary, subjects with low coronary ostia and small aortic root could face more risks and
procedural difficulties in view of a future TAVR-in-TAVR; therefore, a SAVR with large valves and
possibility of aortic root enlargement should be offered, always considering a possible future TAVR-in-
SAVR and, theoretically, a possible TAVR-in-TAVR-in-SAVR .
[64]
As the number of TAVR implants increases, surgical TAVR explantations are also on the rise. From
currently available data, the clinical effects of explant of chronically implanted TAVR with potential need
for aortic repair are not negligible and should be considered in the lifelong management of patient with
aortic stenosis [66,67] . If the adverse outcomes are confirmed over the next few years, TAVR should not be
performed as a first intervention in patients in whom TAVR explantation will be the only possible future
reintervention. However, TAVR explant will remain the primary therapy in patients with THV