Page 14 - Read Online
P. 14
Page 6 of 12 Miller et al. Mini-invasive Surg 2021;5:24 https://dx.doi.org/10.20517/2574-1225.2021.25
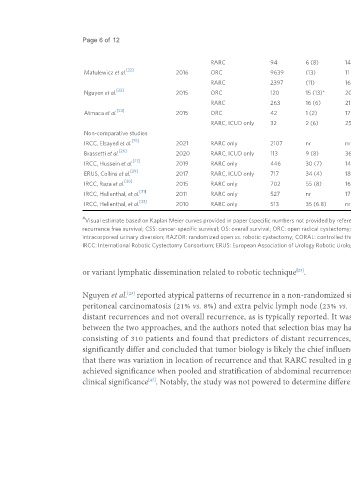
RARC 94 6 (8) 14.9 (SD 10.0) 79%, 2 yr 84%, 2 yr 84%, 2 yr
[22]
Matulewicz et al. 2016 ORC 9639 (13) 11 (IQR 5-19)* nr nr nr
RARC 2397 (11) 16 (IQR 9-25) nr nr nr
[23] #
Nguyen et al. 2015 ORC 120 15 (13)* 20 (IQR 11-27) 60%, 5 yr nr nr
#
RARC 263 16 (6) 21 (IQR 13-28) 70%, 5 yr nr nr
[24]
Atmaca et al. 2015 ORC 42 1 (2) 17 (SD 13.5) nr nr nr
RARC, ICUD only 32 2 (6) 25 (SD 9.7) nr nr nr
Non-comparative studies
[25]
IRCC, Elsayed et al. 2021 RARC only 2107 nr nr 66%, 5 yr nr 60%, 5 yr
[26]
Brassetti et al. 2020 RARC, ICUD only 113 9 (8) 36 (IQR 28-45) 58%, 5 yr 61%, 5 yr 54%, 5 yr
[27]
IRCC, Hussein et al. 2019 RARC only 446 30 (7) 14 (IQR 9-22) 59%, 10 yr 65%, 10 yr 35%, 10 yr
[29]
ERUS, Collins et al. 2017 RARC, ICUD only 717 34 (4) 18 (IQR 13-25) 75%, 2 yr
[30]
IRCC, Raza et al. 2015 RARC only 702 55 (8) 16 (IQR 10-24) 67%, 5 yr 75%, 5 yr 50%, 5 yr
[31]
IRCC, Hellenthal, et al. 2011 RARC only 527 nr 17.8 (range 0-68) nr nr nr
[32]
IRCC, Hellenthal, et al. 2010 RARC only 513 35 (6.8) nr nr nr nr
# *
Visual estimate based on Kaplan Meier curves provided in paper (specific numbers not provided by reference in text). P < 0.05. PSM: Positive surgical margin; SD: standard deviation; IQR: interquartile range; RFS:
recurrence free survival; CSS: cancer-specific survival; OS: overall survival; ORC: open radical cystectomy; RARC: robotic assisted radical cystectomy; LRC: laparoscopic radical cystectomy; nr: not reported; ICUD:
intracorporeal urinary diversion; RAZOR: randomized open vs. robotic cystectomy; CORAL: controlled three-arm trial of open, robotic, and laparoscopic radical cystectomy; RACE: radical cystectomy evaluation;
IRCC: International Robotic Cystectomy Consortium; ERUS: European Association of Urology Robotic Urology Section.
or variant lymphatic dissemination related to robotic technique .
[23]
Nguyen et al. reported atypical patterns of recurrence in a non-randomized single center comparative study of ORC vs. RARC, including higher incidence of
[23]
peritoneal carcinomatosis (21% vs. 8%) and extra pelvic lymph node (23% vs. 15%) [Table 3]. However, the denominator of these estimated proportions was
distant recurrences and not overall recurrence, as is typically reported. It was additionally notable that distant recurrences were not significantly different
between the two approaches, and the authors noted that selection bias may have contributed to these findings. The same group published a follow up study
consisting of 310 patients and found that predictors of distant recurrences, peritoneal carcinomatosis and extra pelvic lymph node metastases did not
[46]
[9]
significantly differ and concluded that tumor biology is likely the chief influencer of atypical recurrence, not surgical approach . Bochner et al. later found
that there was variation in location of recurrence and that RARC resulted in greater numbers of recurrences in the abdomen and pelvis. However, this only
achieved significance when pooled and stratification of abdominal recurrences as separate from distant and local recurrences is controversial and of unclear
[47]
clinical significance . Notably, the study was not powered to determine differences in patterns of recurrence.