Page 42 - Read Online
P. 42
Abdalla et al. Mini-invasive Surg 2019;3:39 I http://dx.doi.org/10.20517/2574-1225.2019.38 Page 9 of 11
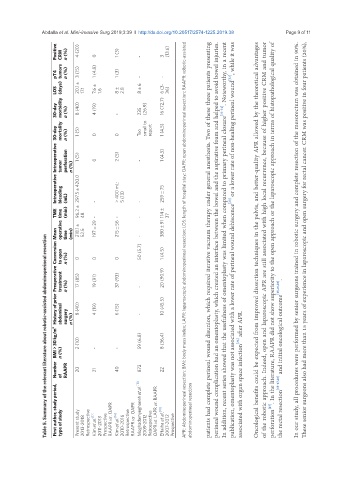
Positive CRM n (%) 4 (20) 0 1 (3) - 3 (13.6)
pT4 tumors n (%) 3 (15) 1 (4.8) 1 (3) - -
LOS (days) 20.1 ± 17.1 7.6 ± 1.6 8 ± 2.8 8 ± 6 6 (3- 36)
30-day morbidity n (%) 8 (40) 4 (19) - 235 (26.9) 16 (72.7)
30-day mortality n (%) 1 (5) 0 0 Too small to report 1 (4.5)
Intraoperative Intraoperative tumor perforation n (%) 1 (5) 297.5 ± 420.0 0 2 (5) > 400 mL: - 1 (4.5)
TME bleeding time operative (mL) (min) time (min) 96.2 ± 218.1 ± 48 52.5 - - 197 ± 29 - 215 ± 56 5 (13) - - - 259 ± 75 114 ± 380 ± 91 37 APR: Abdominoperineal resection; BMI: body mass index; LAPR: laparoscopic abdominoperineal resection; LOS: length of hospital stay; OAPR: open abdominoperineal resection; RAAPR: robotic-assisted patients had complete perineal wound disunion, which required iterative vacuum therapy under g
History of prior Preoperative Conversion Mean to open treatment n (%) n (%) 0 17 (85) 8 (40) 0 19 (91) 4 (19) 0 37 (93) 50 (5.7) - 1 (4.5) 20 (90.9) 10 (45.5)
Table 5. Summary of the relevant literature about robotic-assisted abdominoperineal resection
BMI > 30 kg/m 2 abdominal n (%) surgery n (%) 2 (10) - 6 (15) - - 59 (6.8) 8 (36.4)
Number of RAAPR 20 21 40 872 22 associated with organ space infection [24] after APR. the rectal resection [15-17,26] and initial oncological outcome [15,16,26] .
First author, study period, type of study Present study 2013-2018 Retrospective Kim et al. [17] 2011-2013 Prospective RAAPR vs. OAPR Kim et al. [16] 2010-2016 Retrospective RAAPR vs. OAPR Moghadamyeghaneh et al. [18] 2009-2012 Retrospective OAPR vs. LAPR vs. RAAPR Eftaiha et al. [19] 2007-2012 Prospective abdominoperineal resection