Page 18 - Read Online
P. 18
Page 4 of 8 Ricciardi et al. Mini-invasive Surg 2020;4:1 I http://dx.doi.org/10.20517/2574-1225.2019.50
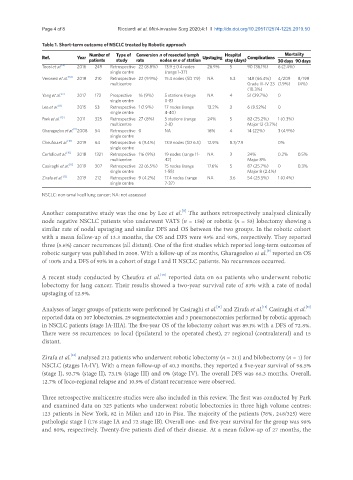
Table 1. Short-term outcome of NSCLC treated by Robotic approach
Number of Type of Conversion n of resected lymph Hospital Mortality
Ref. Year patients study rate nodes or n of station Upstaging stay (days) Complications 30 days 90 days
Toosi et al. [6] 2016 249 Retrospective 22 (8.8%) 13.9 ± 0.4 nodes 26.9% 5 90 (36.1%) 6 (2.4%)
single centre (range 1-37)
Veronesi et al. [14] 2018 210 Retrospective 22 (9.9%) 15.4 nodes (SD 7.9) NA 5.3 148 (66.4%) 4/209 8/198
multicentre Grade III-IV 23 (1.9%) (4%)
(10.3%)
Yang et al. [7] 2017 172 Prospective 16 (9%) 5 stations (range NA 4 51 (29.7%) 0
single centre 0-8)
Lee et al. [8] 2015 53 Retrospective 1 (1.9%) 17 nodes (range 13.2% 3 6 (9.52%) 0
single centre 4-40)
Park et al. [13] 2011 325 Retrospective 27 (8%) 5 stations (range 24% 5 82 (25.2%) 1 (0.3%)
multicentre 2-8) Major 12 (3.7%)
[9]
Gharagozloo et al. 2008 54 Retrospective 0 NA 16% 4 14 (22%) 3 (4.9%)
single centre
Cheufou et al. [10] 2019 64 Retrospective 6 (9.4%) 13.9 nodes (SD 6.5) 12.9% 8.3/7.9 0%
single centre
Cerfolio et al. [15] 2018 1321 Retrospective 116 (9%) 19 nodes (range 11- NA 3 24% 0.2% 0.5%
multicentre 42) Major 8%
Casiraghi et al. [11] 2019 307 Retrospective 22 (6.5%) 15 nodes (range 17.6% 5 87 (25.7%) 0 0.3%
single centre 1-55) Major 8 (2.4%)
Zirafa et al. [12] 2019 212 Retrospective 9 (4.2%) 17.4 nodes (range NA 3.6 54 (25.5%) 1 (0.4%)
single centre 7-37)
NSCLC: non-small-cell lung cancer; NA: not assessed
[8]
Another comparative study was the one by Lee et al. The authors retrospectively analysed clinically
node negative NSCLC patients who underwent VATS (n = 158) or robotic (n = 53) lobectomy showing a
similar rate of nodal upstaging and similar DFS and OS between the two groups. In the robotic cohort
with a mean follow-up of 13.3 months, the OS and DFS were 95% and 93%, respectively. They reported
three (5.6%) cancer recurrences (all distant). One of the first studies which reported long-term outcomes of
robotic surgery was published in 2008. With a follow-up of 28 months, Gharagozloo et al. reported an OS
[9]
of 100% and a DFS of 93% in a cohort of stage I and II NSCLC patients. No recurrences occurred.
[10]
A recent study conducted by Cheufou et al. reported data on 64 patients who underwent robotic
lobectomy for lung cancer. Their results showed a two-year survival rate of 83% with a rate of nodal
upstaging of 12.9%.
[11]
[11]
[12]
Analyses of larger groups of patients were performed by Casiraghi et al. and Zirafa et al. Casiraghi et al.
reported data on 307 lobectomies, 29 segmentectomies and 3 pneumonectomies performed by robotic approach
in NSCLC patients (stage IA-IIIA). The five-year OS of the lobectomy cohort was 89.1% with a DFS of 72.8%.
There were 58 recurrences: 16 local (ipsilateral to the operated chest), 27 regional (contralateral) and 15
distant.
[12]
Zirafa et al. analysed 212 patients who underwent robotic lobectomy (n = 211) and bilobectomy (n = 1) for
NSCLC (stages IA-IV). With a mean follow-up of 40.3 months, they reported a five-year survival of 98.5%
(stage I), 93.7% (stage II), 73.1% (stage III) and 0% (stage IV). The overall DFS was 66.3 months. Overall,
12.7% of loco-regional relapse and 10.9% of distant recurrence were observed.
Three retrospective multicentre studies were also included in this review. The first was conducted by Park
and examined data on 325 patients who underwent robotic lobectomies in three high volume centres:
123 patients in New York, 82 in Milan and 120 in Pisa. The majority of the patients (76%, 248/325) were
pathologic stage I (176 stage IA and 72 stage IB). Overall one- and five-year survival for the group was 98%
and 80%, respectively. Twenty-five patients died of their disease. At a mean follow-up of 27 months, the