Page 47 - Read Online
P. 47
Page 4 of 11 Sullivan et al. Mini-invasive Surg 2023;7:15 https://dx.doi.org/10.20517/2574-1225.2022.106
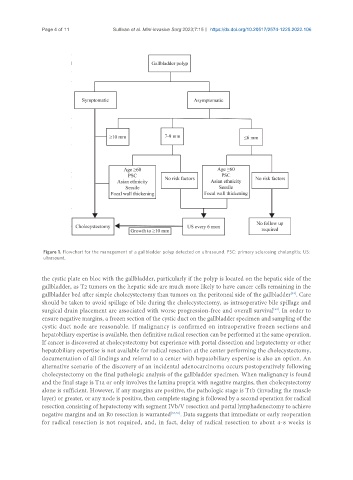
Figure 1. Flowchart for the management of a gallbladder polyp detected on ultrasound. PSC: primary sclerosing cholangitis; US:
ultrasound.
the cystic plate en bloc with the gallbladder, particularly if the polyp is located on the hepatic side of the
gallbladder, as T2 tumors on the hepatic side are much more likely to have cancer cells remaining in the
gallbladder bed after simple cholecystectomy than tumors on the peritoneal side of the gallbladder . Care
[32]
should be taken to avoid spillage of bile during the cholecystectomy, as intraoperative bile spillage and
surgical drain placement are associated with worse progression-free and overall survival . In order to
[33]
ensure negative margins, a frozen section of the cystic duct on the gallbladder specimen and sampling of the
cystic duct node are reasonable. If malignancy is confirmed on intraoperative frozen sections and
hepatobiliary expertise is available, then definitive radical resection can be performed at the same operation.
If cancer is discovered at cholecystectomy but experience with portal dissection and hepatectomy or other
hepatobiliary expertise is not available for radical resection at the center performing the cholecystectomy,
documentation of all findings and referral to a center with hepatobiliary expertise is also an option. An
alternative scenario of the discovery of an incidental adenocarcinoma occurs postoperatively following
cholecystectomy on the final pathologic analysis of the gallbladder specimen. When malignancy is found
and the final stage is T1a or only involves the lamina propria with negative margins, then cholecystectomy
alone is sufficient. However, if any margins are positive, the pathologic stage is T1b (invading the muscle
layer) or greater, or any node is positive, then complete staging is followed by a second operation for radical
resection consisting of hepatectomy with segment IVb/V resection and portal lymphadenectomy to achieve
negative margins and an R0 resection is warranted [34,35] . Data suggests that immediate or early reoperation
for radical resection is not required, and, in fact, delay of radical resection to about 4-8 weeks is