Page 92 - Read Online
P. 92
Page 190 Ma et al. J Transl Genet Genom 2022;6:179-203 https://dx.doi.org/10.20517/jtgg.2021.48
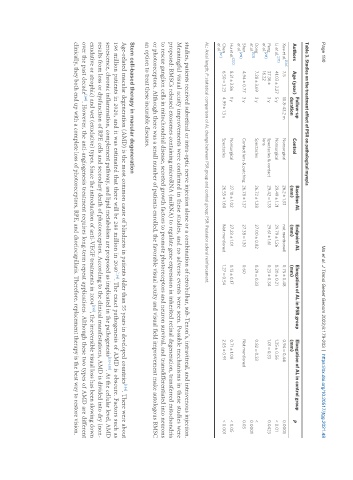
Table 3. Studies on the treatment effect of PSR on pathological myopia
Follow-up Baseline AL Endpoint AL Elongation of AL in PSR group Elongation of AL in control group
Authors Age (year) Control P
duration (mm) (mm) (mm) (mm)
[124]
Xue et al. 7.5 10.8-43.2 m Nonsurgical 26.2 ± 1.33 not mentioned 0.75 ± 0.48 0.94 ± 0.44 0.0001
[217]
Li et al. 41.03 ± 2.27 5 y Nonsurgical 29.49 ± 1.21 29.79 ± 1.26 0.30 ± 0.21 1.35 ± 0.56 < 0.01
Peng 37.36 ± 3 y Spectacles & contact 29.42 ± 1.35 29.61 ± 1.61 0.23 ± 0.34 1.01 ± 0.33 0.0423
[218]
et al. 16.22 lens
Dong 7.28 ± 3.69 3 y Spectacles 26.72 ± 1.28 27.00 ± 0.82 0.29 ± 0.33 0.82 ± 0.33 <
[123]
et al. 0.0001
Shen 4.94 ± 0.77 3 y Contact lens & patching 26.78 ± 1.37 27.38 ± 1.30 0.60 Not mentioned 0.03
[219]
et al.
[220]
Hu et al. 8.21 ± 3.86 1 y Nonsurgical 27.10 ± 1.02 27.23 ± 1.01 0.13 ± 0.17 0.71 ± 1.08 < 0.05
Chen 6.50 ± 3.23 4.99 ± 1.3 y Spectacles 26.55 ± 1.60 Not mentioned 1.27 ± 0.54 2.05 ± 0.91 < 0.001
[121]
et al.
AL: Axial length; P: statistical comparison of AL change between PSR group and control group; PSR: Posterior scleral reinforcement.
studies, patients received subretinal or intra-optic nerve injection alone or a combination of retrobulbar, sub-Tenon’s, intravitreal, and intravenous injection.
Meaningful visual acuity improvements were confirmed in these studies, and no adverse events were seen. Possible mechanisms in these studies were
proposed: BMSCs released exosomes containing microRNA (miRNA) to regulate gene expression in inherited retinal degeneration, transferred mitochondria
to rescue ganglion cells in mitochondrial disease, secreted growth factors to promote photoreceptors and neuron survival, and transdifferentiated into neurons
or photoreceptors. Although there was a small number of patients enrolled, the favorable visual acuity and visual field improvement make autologous BMSC
an option to treat these incurable diseases.
Stem cell-based therapy in macular degeneration
[154]
Age-related macular degeneration (AMD) is the most common cause of blindness in patients older than 55 years in developed countries . There were about
196 million patients in 2020, and it was estimated that there will be 288 million in 2040 . The exact pathogenesis of AMD is obscure. Factors such as
[154]
senescence, chronic inflammation, complement pathway, and lipid metabolism are proposed as implicated in the pathogenesis [155-158] . At the cellular level, AMD
results from loss or dysfunction of RPE cells and secondary death of photoreceptors. According to the clinical manifestations, AMD is divided into dry (non-
[159]
exudative or atrophic) and wet (exudative) types. Since the introduction of anti-VEGF treatments in 2004 , the irreversible visual loss has been slowing down
over the past decade . However, the anti-angiogenesis treatment requires long-term repeat applications. Although these two types of AMD are different
[160]
clinically, they both end up with a complete loss of photoreceptors, RPE, and choriocapillaris. Therefore, replacement therapy is the best way to restore vision.