Page 123 - Read Online
P. 123
Musumeci et al. J Transl Genet Genom 2020;4:221-37 I https://doi.org/10.20517/jtgg.2020.22 Page 227
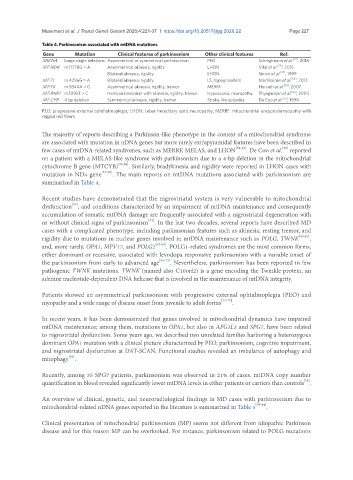
Table 4. Parkinsonism associated with mtDNA mutations
Gene Mutation Clinical features of parkinsonism Other clinical features Ref.
MtDNA Large single deletions Asymmetrical or symmetrical parkinsonism PEO Schreglmann et al. [14] , 2018
MT-ND4 m.11778G > A Asymmetrical akinesia, rigidity LHON Vital et al. [58] , 2015
Bilateral akinesia, rigidity LHON Simon et al. [57] , 1999
MT-TI m.4296G > A Bilateral akinesia, rigidity LS, hypogonadism Martikainen et al. [54] , 2013
MT-TK m.8344A > G Asymmetrical akinesia, rigidity, tremor MERRF Horvath et al. [53] , 2007
MT-RNR1 m.1095T > C Hemiparkinsonism with akinesia, rigidity, tremor Hypoacusia, neuropathy Thyagarajan et al. [52] , 2000
MT-CYB 4 bp deletion Symmetrical akinesia, rigidity, tremor Stroke-like episodes De Coo et al. [55] , 1999
PEO: progressive external ophthalmoplegia; LHON: Leber hereditary optic neuropathy; MERRF: mitochondrial encephalomyopathy with
ragged red fibers
The majority of reports describing a Parkinson-like phenotype in the context of a mitochondrial syndrome
are associated with mutation in nDNA genes but more rarely extrapyramidal features have been described in
few cases of mtDNA-related syndromes, such as MERRF, MELAS, and LHON [52-54] . De Coo et al. reported
[55]
on a patient with a MELAS-like syndrome with parkinsonism due to a 4-bp deletion in the mitochondrial
cytochrome B gene (MTCYB) [55,56] . Similarly, bradykinesia and rigidity were reported in LHON cases with
mutation in ND4 gene [57,58] . The main reports on mtDNA mutations associated with parkinsonism are
summarized in Table 4.
Recent studies have demonstrated that the nigrostriatal system is very vulnerable to mitochondrial
[59]
dysfunction , and conditions characterized by an impairment of mtDNA maintenance and consequently
accumulation of somatic mtDNA damage are frequently associated with a nigrostriatal degeneration with
[14]
or without clinical signs of parkinsonism . In the last two decades, several reports have described MD
cases with a complicated phenotype, including parkinsonian features such as akinesia, resting tremor, and
rigidity due to mutations in nuclear genes involved in mtDNA maintenance such as POLG, TWNK [60,61] ,
and, more rarely, OPA1, MPV17, and POLG2 [62-64] . POLG1-related syndromes are the most common forms,
either dominant or recessive, associated with levodopa responsive parkinsonism with a variable onset of
the parkinsonism from early to advanced age [65-73] . Nevertheless, parkinsonism has been reported in few
pathogenic TWNK mutations. TWNK (named also C10orf2) is a gene encoding the Twinkle protein, an
adenine nucleotide-dependent DNA helicase that is involved in the maintenance of mtDNA integrity.
Patients showed an asymmetrical parkinsonism with progressive external ophtalmoplegia (PEO) and
myopathy and a wide range of disease onset from juvenile to adult forms [74-77] .
In recent years, it has been demonstrated that genes involved in mitochondrial dynamics have impaired
mtDNA maintenance; among them, mutations in OPA1, but also in AFG3L2 and SPG7, have been related
to nigrostriatal dysfunction. Some years ago, we described two unrelated families harboring a heterozygous
dominant OPA1 mutation with a clinical picture characterized by PEO, parkinsonism, cognitive impairment,
and nigrostriatal dysfunction at DAT-SCAN. Functional studies revealed an imbalance of autophagy and
mitophagy .
[62]
Recently, among 35 SPG7 patients, parkinsonism was observed in 21% of cases. mtDNA copy number
[78]
quantification in blood revealed significantly lower mtDNA levels in either patients or carriers than controls .
An overview of clinical, genetic, and neuroradiological findings in MD cases with parkinsonism due to
mitochondrial-related nDNA genes reported in the literature is summarized in Table 5 [79-84] .
Clinical presentation of mitochondrial parkinsonism (MP) seems not different from idiopathic Parkinson
disease and for this reason MP can be overlooked. For instance, parkinsonism related to POLG mutations