Page 45 - Read Online
P. 45
Page 6 of 23 Koukourakis et al. J Cancer Metastasis Treat 2022;8:38 https://dx.doi.org/10.20517/2394-4722.2022.43
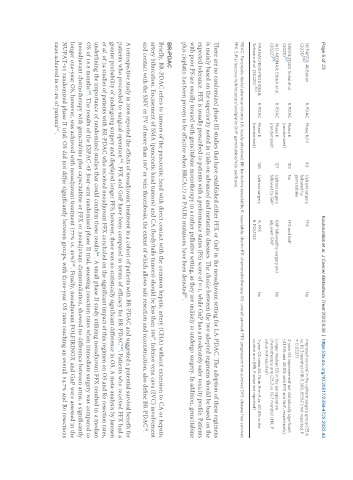
NEPAFOX; Al-Batran R-PDAC Phase II/III 40 Upfront surgery FFX No Improved survival in the upfront surgery group (25.6
[56]
(2021) followed by vs. 10.3 months) (HR 0.366, 95%CI: not reported, P
gemcitabine = 0.0337)
SWOG S1505; Sohal et al. R-PDAC Phase II 103 No FFX and GnP 2-year OS improvement not statistically significant
[57]
(2020) (randomized) (41.6% and 48.8% with FFX and GnP, respectively)
AIO-NEONAX; Ettrich et al. R-PDAC Phase II 127 Upfront surgery GnP followed by surgery and No Longer median OS in the perioperative
[59]
(2022) (randomized) followed by GnP adjuvant GNP chemotherapy arm (25.2 vs. 16.7 months) (HR, P
value not reported)
PAANACHE01-PRODIGE48; R-PDAC Phase II 146 Upfront surgery A. FFX No 1-year OS rates 84.1% in Arm A vs. 80.8% in the
Schwarz et al. (20220) [60] (randomized) B. FOLFOX control arm (HR, P value not reported)
PDAC: Pancreatic ductal adenocarcinoma; LA: locally advanced; BR: borderline resectable; R: resectable; chemo-RT: chemoradiotherapy; OS: overall survival; PFS: progression free survival; DFS: disease free survival;
FFX: 5-FU/leucovorin/irinotecan/oxaliplatin; GnP: gemcitabine/nab-paclitaxel.
There are no randomized phase III studies that have established either FFX or GnP in the neoadjuvant setting for LA-PDAC. The adoption of these regimens
is mainly based on the superiority noted in trials on advanced and metastatic diseases. The choice between the two adopted regimens should be based on the
expected tolerance. FFX is usually prescribed to patients with a performance status (PS) score of 0-1, while GnP has a moderately safer toxicity profile. Patients
with poor PS are usually treated with gemcitabine monotherapy in a rather palliative setting, as they are unlikely to undergo surgery. In addition, gemcitabine
plus cisplatin has been proven to be effective when BRCA1/2 or PALB2 mutations have been detected .
[6]
BR-PDAC
Briefly, BR-PDAC refers to tumors of the pancreatic head with direct contact with the common hepatic artery (CHA) without extension to CA or hepatic
artery bifurcation. Encasement of SMA (pancreatic head tumors) and CA (body/tails tumors) should be less than 180°. Inferior vena cava (IVC) involvement
and contact with the SMV or PV of more than 180° or vein thrombosis, the extent of which allows safe resection and reconstruction, also define BR-PDAC .
[6]
A retrospective study in 2008 reported the effects of neoadjuvant treatment in a cohort of patients with BR-PDAC and suggested a potential survival benefit for
patients who proceeded to surgical operation . FFX and GnP have been compared in terms of efficacy for BR-PDAC . Patients who received FFX had a
[43]
[42]
greater probability of undergoing surgery and displayed longer PFS; however, there was no statistically significant difference in OS. A meta-analysis by Janssen
et al. of 24 studies of patients with BR-PDAC who received neoadjuvant FFX concluded on the significant impact of this regimen on OS and R0 resection rates,
underlining the importance of randomized studies that could confirm these results . A small phase II study utilizing neoadjuvant FFX resulted in a median
[44]
OS of 16.8 months . The results of the ESPAC-5F four-arm randomized phase II trial, assessing resection rates when immediate surgery was compared to
[45]
neoadjuvant chemotherapy with gemcitabine plus capecitabine or FFX or neoadjuvant chemoradiation, showed no difference between arms; a significantly
[46]
longer one-year OS, however, was achieved with neoadjuvant treatment (77% vs. 40%) . Finally, neoadjuvant FOLFIRINOX and GnP were assessed in the
NUPAT-01 randomized phase II trial. OS did not differ significantly between groups, with three-year OS rates reaching an overall 54.7% and R0 resections
rates achieved in 67.4% of patients .
[47]