Page 176 - Read Online
P. 176
Page 4 of 16 Borzio et al. Hepatoma Res 2019;5:15 I http://dx.doi.org/10.20517/2394-5079.2019.11
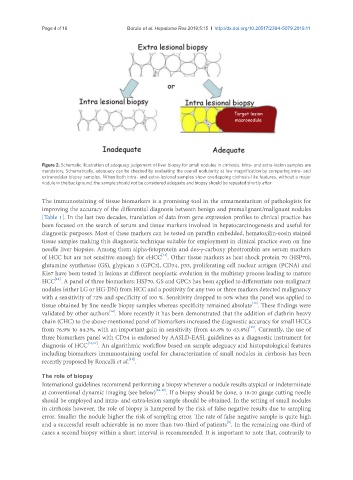
Figure 2. Schematic illustration of adequacy judgement of liver biopsy for small nodules in cirrhosis. Intra- and extra-lesion samples are
mandatory. Schematically, adequacy can be checked by evaluating the overall nodularity at low magnification by comparing intra- and
extranodular biopsy samples. When both intra- and extra-lesional samples show overlapping cirrhosis-like features, without a major
nodule in the background, the sample should not be considered adequate and biopsy should be repeated shortly after
The immunostaining of tissue biomarkers is a promising tool in the armamentarium of pathologists for
improving the accuracy of the differential diagnosis between benign and premalignant/malignant nodules
[Table 1]. In the last two decades, translation of data from gene expression profiles to clinical practice has
been focused on the search of serum and tissue markers involved in hepatocarcinogenesis and useful for
diagnostic purposes. Most of these markers can be tested on paraffin embedded, hematoxilin-eosin stained
tissue samples making this diagnostic technique suitable for employment in clinical practice even on fine
needle liver biopsies. Among them alpha-fetoprotein and des-g-carboxy phrotrombin are serum markers
[12]
of HCC but are not sensitive enough for eHCC . Other tissue markers as heat shock protein 70 (HSP70),
glutamine synthetase (GS), glypican 3 (GPC3), CD34, p53, proliferating cell nuclear antigen (PCNA) and
Ki67 have been tested in lesions at different neoplastic evolution in the multistep process leading to mature
[12]
HCC . A panel of three biomarkers: HSP70, GS and GPC3 has been applied to differentiate non-malignant
nodules (either LG or HG-DN) from HCC and a positivity for any two or three markers detected malignancy
with a sensitivity of 72% and specificity of 100 %. Sensitivity dropped to 50% when the panel was applied to
tissue obtained by fine needle biopsy samples whereas specificity remained absolute . These findings were
[13]
[14]
validated by other authors . More recently it has been demonstrated that the addition of clathrin heavy
chain (CHC) to the above-mentioned panel of biomarkers increased the diagnostic accuracy for small HCCs
[15]
from 76.9% to 84.3%, with an important gain in sensitivity (from 46.8% to 63.8%) . Currently, the use of
three biomarkers panel with CD34 is endorsed by AASLD-EASL guidelines as a diagnostic instrument for
diagnosis of HCC [16,17] . An algorithmic workflow based on sample adeguacy and histopatological features
including biomarkers immunostaining useful for characterization of small nodules in cirrhosis has been
[11]
recently proposed by Roncalli et al. .
The role of biopsy
International guidelines recommend performing a biopsy whenever a nodule results atypical or indeterminate
at conventional dynamic imaging (see below) [16-20] . If a biopsy should be done, a 18-20 gauge cutting needle
should be employed and intra- and extra-lesion sample should be obtained. In the setting of small nodules
in cirrhosis however, the role of biopsy is hampered by the risk of false negative results due to sampling
error. Smaller the nodule higher the risk of sampling error. The rate of false negative sample is quite high
[8]
and a successful result achievable in no more than two-third of patients . In the remaining one-third of
cases a second biopsy within a short interval is recommended. It is important to note that, contrarily to