Page 282 - Read Online
P. 282
Ratti et al. Fast-track management in patients with HCC
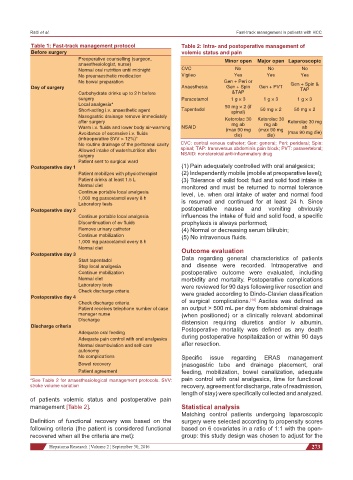
Table 1: Fast-track management protocol Table 2: Intra- and postoperative management of
Before surgery volemic status and pain
Preoperative counselling (surgeon, Minor open Major open Laparoscopic
anaesthesiologist, nurse)
Normal oral nutrition until midnight CVC No No No
No preanaesthetic medication Vigileo Yes Yes Yes
No bowel preparation Gen + Peri or Gen + Spin &
Day of surgery Anaesthesia Gen + Spin Gen + PVT TAP
Carbohydrate drinks up to 2 h before &TAP
surgery Paracetamol 1 g × 3 1 g × 3 1 g × 3
Local analgesia* 50 mg × 2 (if
Short-acting i.v. anaesthetic agent Tapentadol spinal) 50 mg × 2 50 mg × 2
Nasogastric drainage remove immediately
after surgery Ketorolac 30 Ketorolac 30 Ketorolac 30 mg
mg ab
mg ab
Warm i.v. fluids and lower body air-warming NSAID (max 90 mg (max 90 mg ab
Avoidance of excessive i.v. fluids die) die) (max 90 mg die)
(intraoperative SVV > 12%)*
No routine drainage of the peritoneal cavity CVC: central venous catheter; Gen: general; Peri: peridural; Spin:
Allowed intake of water/nutrition after spinal; TAP: transversus abdominis pain block; PVT: paravertebral;
surgery NSAID: nonsteroidal anti-inflammatory drug
Patient sent to surgical ward
Postoperative day 1 (1) Pain adequately controlled with oral analgesics;
Patient mobilizes with physiotherapist (2) Independently mobile (mobile at preoperative level);
Patient drinks at least 1.5 L (3) Tolerance of solid food: fluid and solid food intake is
Normal diet monitored and must be returned to normal tolerance
Continue portable local analgesia level, i.e. when oral intake of water and normal food
1,000 mg paracetamol every 8 h
Laboratory tests is resumed and continued for at least 24 h. Since
Postoperative day 2 postoperative nausea and vomiting obviously
Continue portable local analgesia influences the intake of fluid and solid food, a specific
Discontinuation of ev fluids prophylaxis is always performed;
Remove urinary catheter (4) Normal or decreasing serum bilirubin;
Continue mobilization (5) No intravenous fluids.
1,000 mg paracetamol every 8 h
Normal diet Outcome evaluation
Postoperative day 3
Start tapentadol Data regarding general characteristics of patients
Stop local analgesia and disease were recorded. Intraoperative and
Continue mobilization postoperative outcome were evaluated, including
Normal diet morbidity and mortality. Postoperative complications
Laboratory tests were reviewed for 90 days following liver resection and
Check discharge criteria were graded according to Dindo-Clavien classification
Postoperative day 4 [14]
Check discharge criteria of surgical complications. Ascites was defined as
Patient receives telephone number of case an output > 500 mL per day from abdominal drainage
manager nurse (when positioned) or a clinically relevant abdominal
Discharge distension requiring diuretics and/or iv albumin.
Discharge criteria Postoperative mortality was defined as any death
Adequate oral feeding
Adequate pain control with oral analgesics during postoperative hospitalization or within 90 days
Normal deambulation and self-care after resection.
autonomy
No complications Specific issue regarding ERAS management
Bowel recovery (nasogastric tube and drainage placement, oral
Patient agreement feeding, mobilization, bowel canalization, adequate
*See Table 2 for anaesthesiological management protocols. SVV: pain control with oral analgesics, time for functional
stroke volume variation recovery, agreement for discharge, rate of readmission,
length of stay) were specifically collected and analyzed.
of patients volemic status and postoperative pain
management [Table 2]. Statistical analysis
Matching control patients undergoing laparoscopic
Definition of functional recovery was based on the surgery were selected according to propensity scores
following criteria (the patient is considered functional based on 6 covariates in a ratio of 1:1 with the open-
recovered when all the criteria are met): group: this study design was chosen to adjust for the
Hepatoma Research ¦ Volume 2 ¦ September 30, 2016 273