Page 117 - Read Online
P. 117
Page 6 of 11 Muñoz-Martínez et al. Hepatoma Res 2022;8:30 https://dx.doi.org/10.20517/2394-5079.2022.22
a
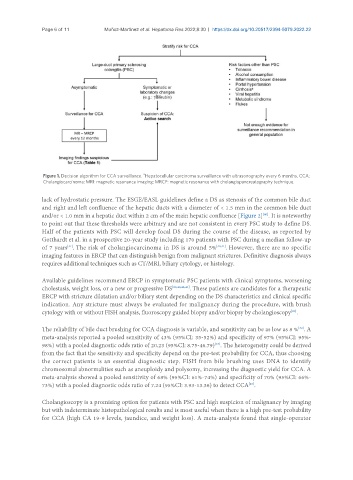
Figure 1. Decision algorithm for CCA surveillance. Hepatocellular carcinoma surveillance with ultrasonography every 6 months. CCA:
Cholangiocarcinoma; MRI: magnetic resonance imaging; MRCP: magnetic resonance with cholangiopancreatography technique.
lack of hydrostatic pressure. The ESGE/EASL guidelines define a DS as stenosis of the common bile duct
and right and left confluence of the hepatic ducts with a diameter of < 1.5 mm in the common bile duct
and/or < 1.0 mm in a hepatic duct within 2 cm of the main hepatic confluence [Figure 2] . It is noteworthy
[40]
to point out that these thresholds were arbitrary and are not consistent in every PSC study to define DS.
Half of the patients with PSC will develop focal DS during the course of the disease, as reported by
Gotthardt et al. in a prospective 20-year study including 170 patients with PSC during a median follow-up
[41]
of 7 years . The risk of cholangiocarcinoma in DS is around 5% [40,41] . However, there are no specific
imaging features in ERCP that can distinguish benign from malignant strictures. Definitive diagnosis always
requires additional techniques such as CT/MRI, biliary cytology, or histology.
Available guidelines recommend ERCP in symptomatic PSC patients with clinical symptoms, worsening
cholestasis, weight loss, or a new or progressive DS [20,40,42,43] . These patients are candidates for a therapeutic
ERCP with stricture dilatation and/or biliary stent depending on the DS characteristics and clinical specific
indication. Any stricture must always be evaluated for malignancy during the procedure, with brush
cytology with or without FISH analysis, fluoroscopy guided biopsy and/or biopsy by cholangioscopy .
[20]
[32]
The reliability of bile duct brushing for CCA diagnosis is variable, and sensitivity can be as low as 8 % . A
meta-analysis reported a pooled sensitivity of 43% (95%CI: 35-52%) and specificity of 97% (95%CI: 95%-
98%) with a pooled diagnostic odds ratio of 20.23 (95%CI: 8.75-46.79) . The heterogeneity could be derived
[44]
from the fact that the sensitivity and specificity depend on the pre-test probability for CCA, thus choosing
the correct patients is an essential diagnostic step. FISH from bile brushing uses DNA to identify
chromosomal abnormalities such as aneuploidy and polysomy, increasing the diagnostic yield for CCA. A
meta-analysis showed a pooled sensitivity of 68% (95%CI: 61%-74%) and specificity of 70% (95%CI: 66%-
[45]
73%) with a pooled diagnostic odds ratio of 7.24 (95%CI: 3.93-13.36) to detect CCA .
Cholangioscopy is a promising option for patients with PSC and high suspicion of malignancy by imaging
but with indeterminate histopathological results and is most useful when there is a high pre-test probability
for CCA (high CA 19-9 levels, jaundice, and weight loss). A meta-analysis found that single-operator