Page 76 - Read Online
P. 76
Calinescu et al. Hepatoma Res 2021;7:59 https://dx.doi.org/10.20517/2394-5079.2021.26 Page 11 of 17
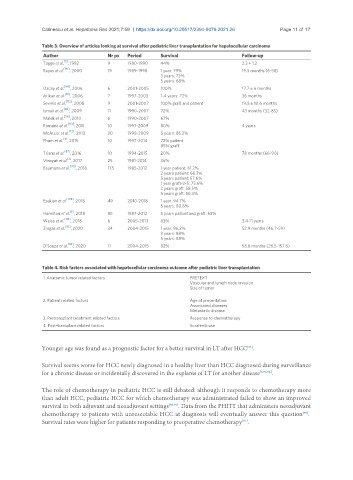
Table 3. Overview of articles looking at survival after pediatric liver transplantation for hepatocellular carcinoma
Author Nr px Period Survival Follow-up
[5]
Tagge et al. , 1992 9 1980-1990 44% 2.3 ± 1.2
[90]
Reyes et al. , 2000 19 1989-1998 1 year: 79% 19.5 months (6-58)
3 years: 73%
5 years: 68%
[94]
Ozcay et al. , 2006 6 2001-2005 100% 17.7 ± 6 months
Arikan et al. [111] , 2006 7 1997-2003 1-4 years: 72% 36 months
[112]
Sevmis et al. , 2008 9 2001-2007 100% graft and patient 19.8 ± 10.6 months
[88]
Ismail et al. , 2009 11 1990-2007 72% 43 months (32-85)
Malek et al. [56] , 2010 6 1990-2007 67%
[113]
Romano et al. , 2011 10 1997-2009 80% 4 years
McAteer et al. [12] , 2013 20 1998-2009 5 years: 85.3%
[4]
Pham et al. , 2015 10 1997-2014 72% patient
85% graft
[87]
Triana et al. , 2016 10 1994-2015 20% 78 months (66-90)
[1]
Vinayak et al. , 2017 25 1981-2014 36%
[93]
Baumann et al. , 2018 175 1985-2012 1 year patient: 81.2%
2 years patient: 68.3%
5 years patient: 57.6%
1 year graft-2-5: 73.6%
2 years graft: 58.5%
5 years graft: 56.3%
Ezekian et al. [108] , 2018 49 2010-2018 1 year: 94.7%
5 years: 80.8%
[8]
Hamilton et al. , 2018 85 1987-2012 5 years patient and graft: 63%
[114]
Weiss et al. , 2018 6 2005-2013 83% 3.4-11 years
Ziogas et al. [92] , 2020 34 2004-2015 1 year: 96.2% 52.9 months (46.7-59)
3 years: 88%
5 years: 88%
[82]
D’Souza et al. , 2020 11 2004-2015 82% 58.8 months (26.5-157.6)
Table 4. Risk factors associated with hepatocellular carcinoma outcome after pediatric liver transplantation
1. Anatomic tumor related factors PRETEXT
Vascular and lymph node invasion
Size of tumor
2. Patient related factors Age at presentation
Associated diseases
Metastatic disease
3. Pretransplant treatment related factors Response to chemotherapy
4. Post-transplant related factors Sorafenib use
Younger age was found as a prognostic factor for a better survival in LT after HCC .
[93]
Survival seems worse for HCC newly diagnosed in a healthy liver than HCC diagnosed during surveillance
for a chronic disease or incidentally discovered in the explants of LT for another disease [3,93,94] .
The role of chemotherapy in pediatric HCC is still debated: although it responds to chemotherapy more
than adult HCC, pediatric HCC for which chemotherapy was administrated failed to show an improved
survival in both adjuvant and neoadjuvant settings [89,92] . Data from the PHITT that administers neoadjuvant
chemotherapy to patients with unresectable HCC at diagnosis will eventually answer this question .
[89]
Survival rates were higher for patients responding to preoperative chemotherapy .
[81]