Page 84 - Read Online
P. 84
Page 8 of 13 Farrell et al. Hepatoma Res 2020;6:18 I http://dx.doi.org/10.20517/2394-5079.2019.019
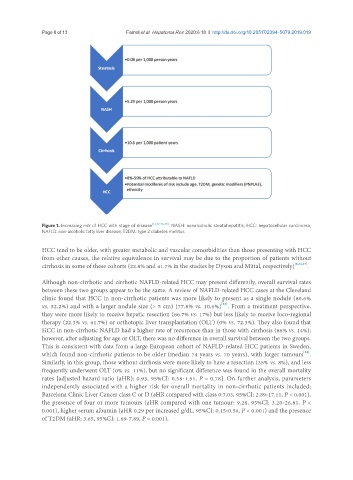
Figure 1. Increasing risk of HCC with stage of disease [1,7,32,36-38] . NASH: nonalcoholic steatohepatitis; HCC: hepatocellular carcinoma;
NAFLD: non-alcoholic fatty liver disease; T2DM: type 2 diabetes mellitus
HCC tend to be older, with greater metabolic and vascular comorbidities than those presenting with HCC
from other causes, the relative equivalence in survival may be due to the proportion of patients without
cirrhosis in some of these cohorts (22.8% and 41.7% in the studies by Dyson and Mittal, respectively) [8,34,37] .
Although non-cirrhotic and cirrhotic NAFLD-related HCC may present differently, overall survival rates
between these two groups appear to be the same. A review of NAFLD-related HCC cases at the Cleveland
clinic found that HCC in non-cirrhotic patients was more likely to present as a single nodule (80.6%
[48]
vs. 52.2%) and with a larger nodule size (> 5 cm) (77.8% vs. 10.6%) . From a treatment perspective,
they were more likely to receive hepatic resection (66.7% vs. 17%) but less likely to receive loco-regional
therapy (22.3% vs. 61.7%) or orthotopic liver transplantation (OLT) (0% vs. 72.3%). They also found that
HCC in non-cirrhotic NAFLD had a higher rate of recurrence than in those with cirrhosis (86% vs. 14%);
however, after adjusting for age or OLT, there was no difference in overall survival between the two groups.
This is consistent with data from a large European cohort of NAFLD-related HCC patients in Sweden,
[52]
which found non-cirrhotic patients to be older (median 74 years vs. 70 years), with larger tumours .
Similarly, in this group, those without cirrhosis were more likely to have a resection (35% vs. 8%), and less
frequently underwent OLT (0% vs. 11%), but no significant difference was found in the overall mortality
rates [adjusted hazard ratio (aHR): 0.93, 95%CI: 0.58-1.51, P = 0.78]. On further analysis, parameters
independently associated with a higher risk for overall mortality in non-cirrhotic patients included;
Barcelona Clinic Liver Cancer class C or D (aHR compared with class 0:7.03, 95%CI: 2.89-17.11, P < 0.001),
the presence of four or more tumours (aHR compared with one tumour: 9.26, 95%CI: 3.20-26.81, P <
0.001), higher serum albumin (aHR 0.29 per increased g/dL, 95%CI: 0.15-0.56, P < 0.001) and the presence
of T2DM (aHR: 3.65, 95%CI: 1.69-7.89, P = 0.001).