Page 12 - Read Online
P. 12
Page 6 of 10 Wang et al. Hepatoma Res 2018;4:14 I http://dx.doi.org/10.20517/2394-5079.2018.16
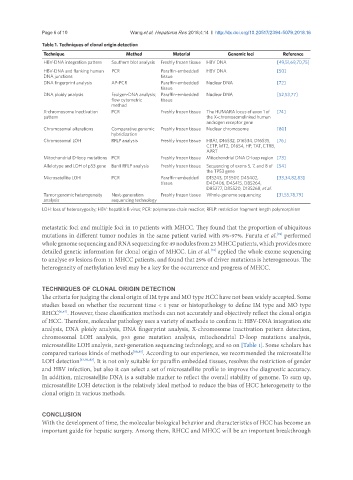
Table 1. Techniques of clonal origin detection
Technique Method Material Genomic loci Reference
HBV-DNA integration pattern Southern blot analysis Freshly frozen tissue HBV DNA [49,51,69,70,75]
HBV-DNA and flanking human PCR Paraffin-embedded HBV DNA [50]
DNA junctions tissue
DNA fingerprint analysis AP-PCR Paraffin-embedded Nuclear DNA [72]
tissue
DNA ploidy analysis Feulgen-DNA analysis; Paraffin-embedded Nuclear DNA [52,53,77]
flow cytometric tissue
method
X-chromosome inactivation PCR Freshly frozen tissue The HUMARA locus of exon 1 of [74]
pattern the X-chromosomelinked human
androgen receptor gene
Chromosomal alterations Comparative genomic Freshly frozen tissue Nuclear chromosome [80]
hybridization
Chromosomal LOH RFLP analysis Freshly frozen tissue HBA1, D16S32, D16S34, D16S35, [76]
CETP, MT2, D16S4, HP, TAT, CTRB,
APRT
Mitochondrial D-loop mutations PCR Freshly frozen tissue Mitochondrial DNA D-loop region [73]
Allelotype and LOH of p53 gene BanII RFLP analysis Freshly frozen tissue Sequencing of exons 5, 7, and 8 of [54]
the TP53 gene
Microsatellite LOH PCR Paraffin-embedded D1S243, D1S507, D4S402, [33,34,82,83]
tissue D4D406, D4S415, D8S264,
D8S277, D8S520, D13S268, et al.
Tumor genomic heterogeneity Next-generation Freshly frozen tissue Whole-genome sequencing [31,55,78,79]
analysis sequencing technology
LOH: loss of heterozygosity; HBV: hepatitis B virus; PCR: polymerase chain reaction; RFLP: restriction fragment length polymorphism
metastatic foci and multiple foci in 10 patients with MHCC. They found that the proportion of ubiquitous
mutations in different tumor nodules in the same patient varied with 8%-97%. Furuta et al. performed
[78]
whole genome sequencing and RNA sequencing for 49 nodules from 23 MHCC patients, which provides more
detailed genetic information for clonal origin of MHCC. Lin et al. applied the whole exome sequencing
[79]
to analyse 69 lesions from 11 MHCC patients, and found that 29% of driver mutations is heterogeneous. The
heterogeneity of methylation level may be a key for the occurrence and progress of MHCC.
TECHNIQUES OF CLONAL ORIGIN DETECTION
The criteria for judging the clonal origin of IM type and MO type HCC have not been widely accepted. Some
studies based on whether the recurrent time < 1 year or histopathology to define IM type and MO type
RHCC [6,47] . However, these classification methods can not accurately and objectively reflect the clonal origin
of HCC. Therefore, molecular pathology uses a variety of methods to confirm it: HBV-DNA integration site
analysis, DNA ploidy analysis, DNA fingerprint analysis, X-chromosome inactivation pattern detection,
chromosomal LOH analysis, p53 gene mutation analysis, mitochondrial D-loop mutations analysis,
microsatellite LOH analysis, next-generation sequencing technology, and so on [Table 1]. Some scholars has
compared various kinds of methods [80,81] . According to our experience, we recommended the microsatellite
LOH detection [33,82,83] . It is not only suitable for paraffin embedded tissues, resolves the restriction of gender
and HBV infection, but also it can select a set of microsatellite profile to improve the diagnostic accuracy.
In addition, microsatellite DNA is a suitable marker to reflect the overall stability of genome. To sum up,
microsatellite LOH detection is the relatively ideal method to reduce the bias of HCC heterogeneity to the
clonal origin in various methods.
CONCLUSION
With the development of time, the molecular biological behavior and characteristics of HCC has become an
important guide for hepatic surgery. Among them, RHCC and MHCC will be an important breakthrough