Page 112 - Read Online
P. 112
Page 58 Ambati et al. Art Int Surg. 2025;5:53-64 https://dx.doi.org/10.20517/ais.2024.45
Table 2. Summary of studies discussed in the intraoperative tools subsection
Area of investigation Selected studies
ML and computer vision tools for optical image-based General technique: Berven et al., 2023 [38]
[39]
intraoperative navigation (reduce radiation exposure) Lumbar degenerative disease: Abdelrahman et al., 2022
[40] [41]
Pediatric deformity: Comstock et al., 2023 ; Lim et al., 2023
[42] [43]
Trauma: Yeretsian et al., 2022 ; Malacon et al., 2022
[44] [45] [46]
Intraoperative AR, VR, and mixed reality tools Eliahu et al., 2022 ; Auloge et al., 2020 ; Burström et al., 2019 ; Elmi-
Terander et al., 2020 [47] ; Charles et al., 2021 [48]
ML: Machine learning; AR: augmented reality; VR: virtual reality.
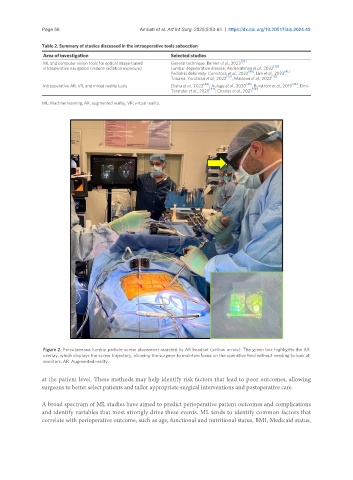
Figure 2. Percutaneous lumbar pedicle screw placement assisted by AR headset (yellow arrow). The green box highlights the AR
overlay, which displays the screw trajectory, allowing the surgeon to maintain focus on the operative field without needing to look at
monitors. AR: Augmented reality.
at the patient level. These methods may help identify risk factors that lead to poor outcomes, allowing
surgeons to better select patients and tailor appropriate surgical interventions and postoperative care.
A broad spectrum of ML studies have aimed to predict perioperative patient outcomes and complications
and identify variables that most strongly drive these events. ML tends to identify common factors that
correlate with perioperative outcome, such as age, functional and nutritional status, BMI, Medicaid status,