Page 59 - Read Online
P. 59
Kimbowa et al. Art Int Surg 2024;4:149-69 https://dx.doi.org/10.20517/ais.2024.20 Page 153
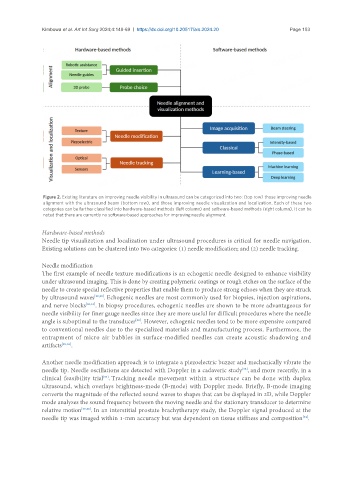
Figure 2. Existing literature on improving needle visibility in ultrasound can be categorized into two: (top row) those improving needle
alignment with the ultrasound beam (bottom row), and those improving needle visualization and localization. Each of these two
categories can be further classified into hardware-based methods (left column) and software-based methods (right column). It can be
noted that there are currently no software-based approaches for improving needle alignment.
Hardware-based methods
Needle tip visualization and localization under ultrasound procedures is critical for needle navigation.
Existing solutions can be clustered into two categories: (1) needle modification; and (2) needle tracking.
Needle modification
The first example of needle texture modifications is an echogenic needle designed to enhance visibility
under ultrasound imaging. This is done by creating polymeric coatings or rough etches on the surface of the
needle to create special reflective properties that enable them to produce strong echoes when they are struck
by ultrasound waves [29,30] . Echogenic needles are most commonly used for biopsies, injection aspirations,
and nerve blocks [30,31] . In biopsy procedures, echogenic needles are shown to be more advantageous for
needle visibility for finer gauge needles since they are more useful for difficult procedures where the needle
angle is suboptimal to the transducer . However, echogenic needles tend to be more expensive compared
[29]
to conventional needles due to the specialized materials and manufacturing process. Furthermore, the
entrapment of micro air bubbles in surface-modified needles can create acoustic shadowing and
artifacts [29,32] .
Another needle modification approach is to integrate a piezoelectric buzzer and mechanically vibrate the
needle tip. Needle oscillations are detected with Doppler in a cadaveric study , and more recently, in a
[33]
clinical feasibility trial . Tracking needle movement within a structure can be done with duplex
[34]
ultrasound, which overlays brightness-mode (B-mode) with Doppler mode. Briefly, B-mode imaging
converts the magnitude of the reflected sound waves to shapes that can be displayed in 2D, while Doppler
mode analyzes the sound frequency between the moving needle and the stationary transducer to determine
relative motion [35,36] . In an interstitial prostate brachytherapy study, the Doppler signal produced at the
needle tip was imaged within 1-mm accuracy but was dependent on tissue stiffness and composition .
[34]