Page 76 - Read Online
P. 76
Page 4 of 7 Rostagno. Vessel Plus 2020;4:7 I http://dx.doi.org/10.20517/2574-1209.2019.29
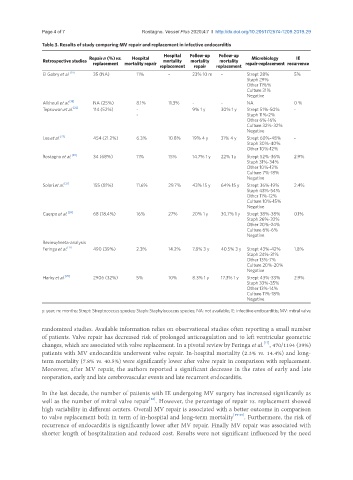
Table 3. Results of study comparing MV repair and replacement in infective endocarditis
Hospital Follow-up Follow-up
Repair n (%) vs. Hospital Microbiology IE
Retrospective studies mortality mortality mortality
replacement mortality repair repair-replacement recurrence
replacement repair replacement
El Gabry et al. [19] 35 (NA) 11% - 23% 10 m - Strept 28% 5%
Staph 29%
Other 11%%
Culture 31%
Negative
Alkhouli et al. [18] NA (25%) 8.1% 11.3% - - NA 0 %
Tepsuwan et al. [22] 114 (52%) - 9% 1 y 30% 1 y Strept 51%-50% -
- Staph 11%-2%
Other 6%-16%
Culture 32%-32%
Negative
Lee et al. [23] 454 (21.2%) 6.3% 10.8% 19% 4 y 31% 4 y Strept 60%-48% -
Staph 30%-40%
Other 10%-12%
Rostagno et al. [20] 34 (68%) 11% 15% 14.7% 1 y 22% 1 y Strept 52%-36% 2.9%
Staph 31%-34%
Other 10%-12%
Culture 7%-18%
Negative
Solari et al. [21] 155 (81%) 11.6% 29.7% 43% 15 y 64% 15 y Strept 36%-19% 2.4%
Staph 43%-54%
Other 11%-12%
Culture 10%-15%
Negative
Cuerpo et al. [24] 68 (18.4%) 16% 27% 20% 1 y 30.7% 1 y Strept 38%-38% 0.1%
Staph 26%-32%
Other 20%-24%
Culture 6%-6%
Negative
Review/meta-analysis
Feringa et al. [17] 490 (39%) 2.3% 14.2% 7.8% 3 y 40.5% 3 y Strept 43%-42% 1.8%
Staph 24%-31%
Other 13%-7%
Culture 20%-20%
Negative
Harky et al. [25] 2906 (32%) 5% 10% 8.3% 1 y 17.3% 1 y Strept 43%-33% 2.9%
Staph 33%-35%
Other 13%-14%
Culture 11%-18%
Negative
y: year; m: months; Strept: Streptococcus species; Staph: Staphylococcus species; NA: not available; IE: infectiive endocarditis; MV: mitral valve
randomized studies. Available information relies on observational studies often reporting a small number
of patients. Valve repair has decreased risk of prolonged anticoagulation and to left ventricular geometric
[17]
changes, which are associated with valve replacement. In a pivotal review by Feringa et al. , 470/1194 (39%)
patients with MV endocarditis underwent valve repair. In-hospital mortality (2.3% vs. 14.4%) and long-
term mortality (7.8% vs. 40.5%) were significantly lower after valve repair in comparison with replacement.
Moreover, after MV repair, the authors reported a significant decrease in the rates of early and late
reoperation, early and late cerebrovascular events and late recurrent endocarditis.
In the last decade, the number of patients with IE undergoing MV surgery has increased significantly as
[18]
well as the number of mitral valve repair . However, the percentage of repair vs. replacement showed
high variability in different centers. Overall MV repair is associated with a better outcome in comparison
to valve replacement both in term of in-hospital and long-term mortality [19-25] . Furthermore, the risk of
recurrence of endocarditis is significantly lower after MV repair. Finally MV repair was associated with
shorter length of hospitalization and reduced cost. Results were not significant influenced by the need