Page 61 - Read Online
P. 61
Harky et al. Vessel Plus 2018;2:8 I http://dx.doi.org/10.20517/2574-1209.2018.12 Page 3 of 7
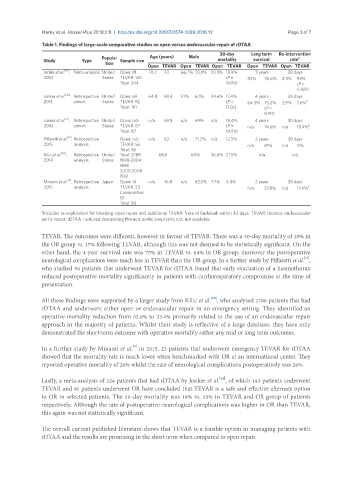
Table 1. Findings of large-scale comparative studies on open versus endovascular repair of rDTAA
Popula- Age (years) Male 30-day Long term Re-intervention
a
Study Type Sample size mortality survival rate
tion
Open TEVAR Open TEVAR Open TEVAR Open TEVAR Open TEVAR
Jonker et al. [18] , Meta-analysis United Open: 81 70.2 70 66.7% 70.8% 33.3% 18.9% 3 years 30 days
2010 States TEVAR: 143 (P = 82% 70.6% 2.3% 9.1%
Total: 244 0.016) (P =
0.169)
Jonker et al. [16] , Retrospective United Open: 69 64.8 69.4 51% 62% 24.6% 17.4% 4 years 30 days
2011 cohort States TEVAR: 92 (P = 64.3% 75.2% 2.9% 7.6% b
Total: 161 0.26) (P =
0.191)
[7]
Jonker et al. , Retrospective United Open: n/a n/a 69.8 n/a 69% n/a 18.4% 4 years 30 days
2010 cohort States TEVAR: 87 (P = n/a 74.6% n/a 18.4% b
Total: 87 0.014)
Piffaretti et al. , Retrospective Open: n/a n/a 62 n/a 71.2% n/a 12.5% 2 years 30 days
[17]
2015 analysis TEVAR: 56 n/a 81% n/a 0%
Total: 56
[15]
Kilic et al. , Retrospective United Total: 2788 68.6 60% 36.6% 21.5% n/a n/a
2014 analysis States 1998-2004:
1596
2005-2008:
1192
Minami et al. , Retrospective Japan Open: 14 n/a 76.8 n/a 62.5% 7.7% 4.3% 2 years 30 days
[8]
2015 analysis TEVAR: 23 n/a 57.8% n/a 17.4% b
Conservative:
13
Total: 50
a Includes re-exploration for bleeding, open repair and additional TEVAR; rate of Endoleak within 30 days. TEVAR: thoracic endovascular
b
aortic repair; rDTAA: ruptured descending thoracic aortic aneurysm; n/a: not available
TEVAR. The outcomes were different, however in favour of TEVAR. There was a 30-day mortality of 25% in
the OR group vs. 17% following TEVAR, although this was not deemed to be statistically significant. On the
other hand, the 4-year survival rate was 75% in TEVAR vs. 64% in OR group; moreover the postoperative
[17]
neurological complications were much less in TEVAR than the OR group. In a further study by Piffaretti et al. ,
who studied 56 patients that underwent TEVAR for rDTAA found that early evacuation of a haemothorax
reduced postoperative mortality significantly in patients with cardiorespiratory compromise at the time of
presentation.
[15]
All these findings were supported by a larger study from Kilic et al. , who analysed 2788 patients that had
rDTAA and underwent either open or endovascular repair in an emergency setting. They identified an
operative mortality reduction from 52.6% to 23.4% primarily related to the use of an endovascular repair
approach in the majority of patients. Whilst their study is reflective of a large database, they have only
demonstrated the short-term outcome with operative mortality rather any mid or long term outcomes.
[8]
In a further study by Minami et al. in 2015, 23 patients that underwent emergency TEVAR for rDTAA
showed that the mortality rate is much lower when benchmarked with OR at an international center. They
reported operative mortality of 26% whilst the rate of neurological complications postoperatively was 26%.
[18]
Lastly, a meta-analysis of 224 patients that had rDTAA by Jonker et al. , of which 143 patients underwent
TEVAR and 81 patients underwent OR have concluded that TEVAR is a safe and effective alternate option
to OR in selected patients. The 30-day mortality was 19% vs. 33% in TEVAR and OR group of patients
respectively. Although the rate of postoperative neurological complications was higher in OR than TEVAR,
this again was not statistically significant.
The overall current published literature shows that TEVAR is a feasible option in managing patients with
rDTAA and the results are promising in the short term when compared to open repair.