Page 88 - Read Online
P. 88
Nardi et al. Postoperative malperfusion in aortic dissection
Table 5: Predictors of late mortality 100
Univariate Multivariate
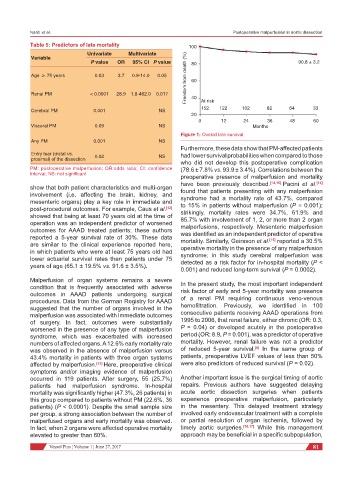
Freedom from death (%) 60
Variable
P value OR 95% CI P value 80 90.8 ± 3.2
Age ≥ 75 years 0.03 3.7 0.9-14.0 0.05
Renal PM < 0.0001 28.9 1.8-462.0 0.017 40 At risk
Cerebral PM 0.001 NS 152 122 102 82 64 33
20
0 12 24 36 48 60
Visceral PM 0.09 NS Months
Figure 1: Overall late survival
Any PM 0.001 NS
Furthermore, these data show that PM-affected patients
Entry tear (distal vs. had lower survival probabilities when compared to those
proximal) of the dissection 0.02 NS
who did not develop this postoperative complication
PM: postoperative malperfusion; OR:odds ratio; CI: confidence (78.6 ± 7.8% vs. 93.9 ± 3.4%). Correlations between the
interval; NS: not significant
preoperative presence of malperfusion and mortality
have been previously described. [14,15] Pacini et al. [14]
show that both patient characteristics and multi-organ found that patients presenting with any malperfusion
involvement (i.e. affecting the brain, kidney, and syndrome had a mortality rate of 43.7%, compared
mesenteric organs) play a key role in immediate and to 15% in patients without malperfusion (P = 0.001);
post-procedural outcomes. For example, Caus et al. [12] strikingly, mortality rates were 34.7%, 61.9% and
showed that being at least 70 years old at the time of 85.7% with involvement of 1, 2, or more than 2 organ
operation was an independent predictor of worsened malperfusions, respectively. Mesenteric malperfusion
outcomes for AAAD treated patients; these authors was identified as an independent predictor of operative
reported a 5-year survival rate of 30%. These data mortality. Similarly, Geirsson et al. [15] reported a 30.5%
are similar to the clinical experience reported here, operative mortality in the presence of any malperfusion
in which patients who were at least 75 years old had syndrome; in this study cerebral malperfusion was
lower actuarial survival rates than patients under 75 detected as a risk factor for in-hospital mortality (P <
years of age (65.1 ± 19.5% vs. 91.6 ± 3.5%).
0.001) and reduced long-term survival (P = 0.0002).
Malperfusion of organ systems remains a severe In the present study, the most important independent
condition that is frequently associated with adverse risk factor of early and 5-year mortality was presence
outcomes in AAAD patients undergoing surgical
procedures. Data from the German Registry for AAAD of a renal PM requiring continuous veno-venous
suggested that the number of organs involved in the hemofiltration. Previously, we identified in 100
malperfusion was associated with immediate outcomes consecutive patients receiving AAAD operations from
of surgery. In fact, outcomes were substantially 1995 to 2006, that renal failure, either chronic (OR: 0.3,
worsened in the presence of any type of malperfusion P = 0.04) or developed acutely in the postoperative
syndrome, which was exacerbated with increased period (OR: 8.9, P = 0.001), was a predictor of operative
numbers of affected organs. A 12.6% early mortality rate mortality. However, renal failure was not a predictor
[8]
was observed in the absence of malperfusion versus of reduced 5-year survival. In the same group of
43.4% mortality in patients with three organ systems patients, preoperative LVEF values of less than 50%
affected by malperfusion. [13] Here, preoperative clinical were also predictors of reduced survival (P = 0.02).
symptoms and/or imaging evidence of malperfusion
occurred in 119 patients. After surgery, 55 (25.7%) Another important issue is the surgical timing of aortic
patients had malperfusion syndrome. In-hospital repairs. Previous authors have suggested delaying
mortality was significantly higher (47.3%, 26 patients) in acute aortic dissection surgeries when patients
this group compared to patients without PM (22.6%, 36 experience preoperative malperfusion, particularly
patients) (P < 0.0001). Despite the small sample size in the mesentery. This delayed treatment strategy
per group, a strong association between the number of involved early endovascular treatment with a complete
malperfused organs and early mortality was observed. or partial resolution of organ ischemia, followed by
In fact, when 2 organs were affected operative mortality timely aortic surgeries. [16,17] While this management
elevated to greater than 60%. approach may be beneficial in a specific subpopulation,
Vessel Plus ¦ Volume 1 ¦ June 27, 2017 81