Page 40 - Read Online
P. 40
Page 6 of 12 Geragotellis et al. Vessel Plus 2023;7:6 https://dx.doi.org/10.20517/2574-1209.2022.41
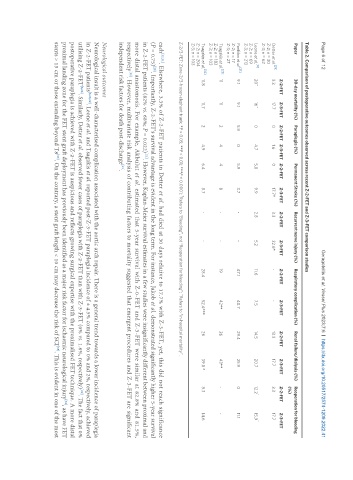
Table 2. Comparison of postoperative outcomes observed across recent Z-2-FET and Z-3-FET comparison studies
Paper 30-day mortality (%) Paraplegia (%) Permanent Stroke (%) Recurrent nerve injury (%) Respiratory complication (%) Renal failure/dialysis (%) Reoperation for bleeding
(%)
Z-2-FET Z-3-FET Z-2-FET Z-3-FET Z-2-FET Z-3-FET Z-2-FET Z-3-FET Z-2-FET Z-3-FET Z-2-FET Z-3-FET Z-2-FET Z-3-FET
[29]
Detter et al. 3.3 17.7 0 1.6 0 17.7* 3.3 22.6* - - 13.3 17.7 3.3 17.7
Z-2; n = 30
Z-3; n = 62
[8]
Leone et al. 20^ 16^ 0 4.7 5.8 9.9 2.8 5.2 11.6 7.5 14.5 20.7 12.2 † 15.9 †
Z-2; n = 69
Z-3; n = 213
[31]
Panfilov et al. 9.1 9.1 5.9 0 5.9 3.7 - - 47.1 40.7 29.4 25.9 0 11.1
Z-2; n = 17
Z-3; n = 27
[28]
Tsagakis et al. 11 11 2 4 4 8 - - 19 42** 26 43** - -
Z-2; n = 183
Z-3; n = 103
Tsagakis et al. [32] 11.8 11.7 2 4.9 6.4 8.7 - - 28.4 52.4*** 26 39.8 * 8.3 14.6
Z-2; n = 204
Z-3; n = 103
†
Z-2/3-FET: Zone-2/3-frozen elephant trunk; *P < 0.05; **P < 0.01; ***P < 0.0001; Refers to “Bleeding”, not “Reoperation for bleeding”; ^Refers to “in-hospital mortality”.
each [32,31] . Elsewhere, 3.3% of Z-2-FET patients in Detter et al. had died at 30 days relative to 17.7% with Z-3-FET, yet, this did not reach significance
[29]
(P = 0.75) . Importantly, Z-2-FET’s survival advantage is evident in the long term. For instance, Jakob et al. demonstrated significantly higher 5-year survival
in Z-2-FET patients (82% vs. 68%; P = 0.022) . However, Kaplan-Meier survival estimates in a few studies were insignificantly different between proximal and
[21]
more distal anastomosis. For example, Akbulut et al. estimated that 5-year survival with Z-0-FET and Z-3-FET were similar at 82.8% and 81.5%,
respectively . However, multivariate risk analysis of contributing factors to mortality suggested that emergent procedures and Z-3-FET are significant
[33]
[21]
independent risk factors for death post-discharge .
Neurological outcomes
Neurological insult is a well-characterised complication associated with the aortic arch repair. There is a general trend towards a lower incidence of paraplegia
in Z-2-FET patients [8,28,29] . Leone et al. and Tsagakis et al. reported post-Z-3-FET paraplegia incidence of ± 4.5% compared to 0% and 2%, respectively, achieved
utilising Z-2-FET [8,28] . Similarly, Detter et al. observed fewer cases of paraplegia with Z-2-FET than with Z-3-FET (0% vs. 1.6%, respectively) . The fact that 0%
[29]
postoperative paraplegia is achieved with Z-2-FET is auspicious and reflects growing surgical expertise with the proximalised FET technique. A more distal
proximal landing zone for the FET stent graft deployment has previously been identified as a major risk factor for ischaemic neurological injury , as have FET
[34]
stents > 15 cm or those extending beyond T8 . On the contrary, a stent graft length < 10 cm may decrease the risk of SCI . This is evident in one of the most
[35]
[35]