Page 39 - Read Online
P. 39
Geragotellis et al. Vessel Plus 2023;7:6 https://dx.doi.org/10.20517/2574-1209.2022.41 Page 5 of 12
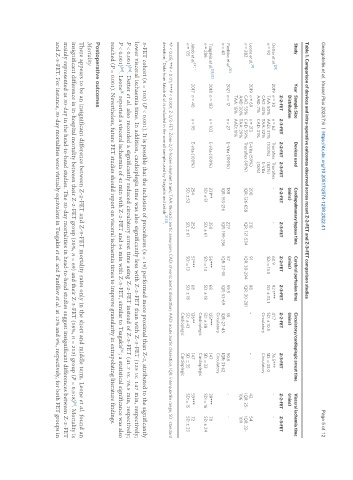
Table 1. Comparison of devices and intra-operative outcomes observed across recent Z-2-FET and Z-3-FET comparison studies
Study Year Sample Size Devices used Cardiopulmonary bypass time Cerebral perfusion time Circulatory/cardioplegic arrest time Visceral ischemia time
Distribution (mins) (mins) (mins) (mins)
Z-2-FET Z-3-FET Z-2-FET Z-3-FET Z-2-FET Z-3-FET Z-2-FET Z-3-FET Z-2-FET Z-3-FET Z-2-FET Z-3-FET
[29]
Detter et al. 2019 n = 30 n = 62 Thoraflex Thoraflex - - 60.9 92.1*** 41.7 76.5*** - -
n = 92 TAA: 50% AAD: 37% (100%) (82%) SD: ± 13.5 SD: ± 33.1 SD: ± 10.5 SD: ± 33.0
CAD: 43% TAA: 32% E-Vita Circulatory Circulatory
AAD: 7% CAD: 31% (18%)
[8]
Leone et al. 2019 n = 69 n = 213 E-Vita (59%) 200 210 91 88 - - 42 54
n = 282 CAD: 55% CAD: 59% Thoraflex (41%) IQR: 126-658 IQR: 121-534 IQR: 30-294 IQR: 30-281 IQR: 25- IQR: 22-
AAD: 30% TAA: 29% 106 109
TAA: 15% AAD: 11%
[31]
Panfilov et al. 2021 n = 17 n = 27 E-Vita (100%) 188 227 57 59.5 35 50.5 - -
n = 43 IQR: 153-216 IQR: 199-256 IQR: 37-91 IQR: 53-69 IQR: 27-45 IQR: 31-62
Circulatory Circulatory
[28,32]
Tsagakis et al. 2018 n = 183 n = 103 E-vita (100%) 231** 250 56*** 68 125*** 147 39*** 70
n = 286 SD: ± 51 SD: ± 61 SD: ± 14 SD: ± 18 SD: ± 38 SD: ± 33 SD: ± 16 SD: ± 24
Cardioplegic Cardioplegic
[21] †
Jakob et al. 2017 n = 40 n = 95 E-vita (100%) 254 252 57*** 68 126** 147 59*** 72
n = 135 SD: ± 52 SD: ± 61 SD: ± 13 SD: ± 18 SD: ± 43 SD: ± 35 SD: ± 15 SD: ± 23
Cardioplegic Cardioplegic
*P < 0.05; **P < 0.01; ***P < 0.001; Z-2/3-FET: Zone-2/3-frozen elephant trunk; TAA: thoracic aortic aneurysm; CAD: chronic aortic dissection; AAD: acute aortic dissection; IQR: interquartile range; SD: standard
† [21,32]
deviation; Data from Jakob et al. is included in the overall sample used by Tsagakis and Jakob .
3-FET cohort (n = 103) (P < 0.001). It is possible that the inclusion of procedures (n = 19) performed more proximal than Z-2, attributed to the significantly
lower visceral ischaemia time. In addition, cardioplegia time was also significantly less with Z-2-FET than with Z-3-FET (125 vs. 147 min, respectively;
P < 0.001) . Detter et al. also recorded a significantly reduced circulatory arrest time using Z-2-FET instead of Z-3-FET (41.7 vs. 76.5 min, respectively;
[32]
P < 0.001) . Leone reported a visceral ischaemia of 42 min with Z-2-FET and 54 min with Z-3-FET, similar to Tsagakis ; a statistical significance was also
[32]
[29]
[8]
reached (P = 0.001). Nevertheless, future FET studies should report on visceral ischaemia times to improve granularity in extrapolating literature findings.
Postoperative outcomes
Mortality
There appears to be an insignificant difference between Z-2-FET and Z-3-FET mortality rates only in the short and middle term. Leone et al. found an
[8]
insignificant difference in in-hospital mortality between their Z-2-FET group (20%, n = 69) and their Z-3-FET (16%, n = 213) group (P = 0.518) . Mortality is
mainly represented as 30-day in the head-to-head studies. The 30-day mortalities in head-to-head studies suggest insignificant differences between Z-2-FET
and Z-3-FET. For instance, 30-day mortalities were virtually equivalent in Tsagakis et al. and Panfilov et al. at 12% and 9%, respectively, for both FET groups in