Page 23 - Read Online
P. 23
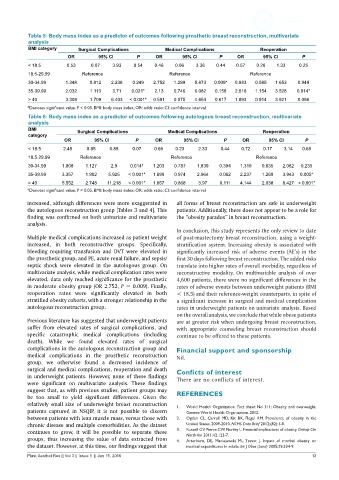
Table 5: Body mass index as a predictor of outcomes following prosthetic breast reconstruction, multivariate
analysis
BMI category Surgical Complications Medical Complications Reoperation
OR 95% CI P OR 95% CI P OR 95% CI P
< 18.5 0.53 0.07 3.93 0.54 0.46 0.06 3.36 0.44 0.57 0.26 1.33 0.25
18.5‑29.99 Reference Reference Reference
30‑34.99 1.348 0.812 2.238 0.249 2.752 1.289 5.873 0.009* 0.983 0.585 1.653 0.949
35‑39.99 2.032 1.113 3.71 0.021* 2.13 0.746 6.082 0.158 2.018 1.154 3.528 0.014*
> 40 3.308 1.709 6.403 < 0.001* 0.591 0.075 4.654 0.617 1.893 0.914 3.921 0.086
*Denotes significant value, P < 0.05. BMI: body mass index; OR: odds ratio; CI: confidence interval
Table 6: Body mass index as a predictor of outcomes following autologous breast reconstruction, multivariate
analysis
BMI Surgical Complications Medical Complications Reoperation
category
OR 95% CI P OR 95% CI P OR 95% CI P
< 18.5 2.48 0.85 6.88 0.07 0.66 0.23 2.33 0.44 0.72 0.17 3.14 0.68
18.5‑29.99 Reference Reference Reference
30‑34.99 1.808 1.127 2.9 0.014* 1.203 0.787 1.839 0.394 1.319 0.835 2.082 0.235
35‑39.99 3.357 1.902 5.925 < 0.001* 1.699 0.974 2.964 0.062 2.237 1.269 3.943 0.005*
> 40 5.552 2.748 11.218 < 0.001* 1.857 0.868 3.97 0.111 4.144 2.038 8.427 < 0.001*
*Denotes significant value, P < 0.05. BMI: body mass index; OR: odds ratio; CI: confidence interval
increased, although differences were more exaggerated in all forms of breast reconstruction are safe in underweight
the autologous reconstruction group [Tables 3 and 4]. This patients. Additionally, there does not appear to be a role for
finding was confirmed on both univariate and multivariate the “obesity paradox” in breast reconstruction.
analysis.
In conclusion, this study represents the only review to date
Multiple medical complications increased as patient weight of post-mastectomy breast reconstruction, using a weight-
increased, in both reconstructive groups. Specifically, stratification system. Increasing obesity is associated with
bleeding requiring transfusion and DVT were elevated in significantly increased risk of adverse events (AE’s) in the
the prosthetic group; and PE, acute renal failure, and sepsis/ first 30 days following breast reconstruction. The added risks
septic shock were elevated in the autologous group. On translate into higher rates of overall morbidity, regardless of
multivariate analysis, while medical complication rates were reconstructive modality. On multivariable analysis of over
elevated, data only reached significance for the prosthetic 4,600 patients, there were no significant differences in the
in moderate obesity group (OR 2.752, P = 0.009). Finally, rates of adverse events between underweight patients (BMI
reoperation rates were significantly elevated in both < 18.5) and their reference-weight counterparts, in spite of
stratified obesity cohorts, with a stronger relationship in the a significant increase in surgical and medical complication
autologous reconstruction group. rates in underweight patients on univariate analysis. Based
on the overall analysis, we conclude that while obese patients
Previous literature has suggested that underweight patients are at greater risk when undergoing breast reconstruction,
suffer from elevated rates of surgical complications, and with appropriate counseling breast reconstruction should
specific catastrophic medical complications (including continue to be offered to these patients.
death). While we found elevated rates of surgical
complications in the autologous reconstruction group and Financial support and sponsorship
medical complications in the prosthetic reconstruction Nil.
group, we otherwise found a decreased incidence of
surgical and medical complications, reoperation and death Conficts of interest
in underweight patients. However, none of these findings There are no conflicts of interest.
were significant on multivariate analysis. These findings
suggest that, as with previous studies, patient groups may
be too small to yield significant differences. Given the REFERENCES
relatively small size of underweight breast reconstruction 1. World Health Organization. Fact sheet No 311: Obesity and overweight.
patients captured in NSQIP, it is not possible to discern Geneva: World Health Organization. 2012.
between patients with lean muscle mass, versus those with 2. Ogden CL, Carroll MD, Kit BK, Flegal KM. Prevalence of obesity in the
chronic disease and multiple comorbidities. As the dataset United States, 2009-2010. NCHS Data Brief 2012;(82):1-8.
continues to grow, it will be possible to separate these 3. Russell GV, Pierce CW, Nunley L. Financial implications of obesity. Orthop Clin
North Am 2011;42:123-7.
groups, thus increasing the value of data extracted from 4. Arterburn, DE, Maciejewski ML Tsevat J. Impact of morbid obesity on
the dataset. However, at this time, our findings suggest that medical expenditures in adults. Int J Obes (Lond) 2005;29:334-9.
Plast Aesthet Res || Vol 3 || Issue 1 || Jan 15, 2016 13