Page 44 - Read Online
P. 44
Page 12 of 17 Garoosi et al. Plast Aesthet Res 2024;11:42 https://dx.doi.org/10.20517/2347-9264.2024.57
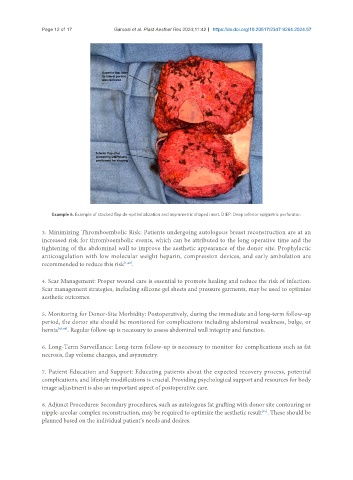
Example 6. Example of stacked flap de-epithelialization and asymmetric shaped inset. DIEP: Deep inferior epigastric perforator.
3. Minimizing Thromboembolic Risk: Patients undergoing autologous breast reconstruction are at an
increased risk for thromboembolic events, which can be attributed to the long operative time and the
tightening of the abdominal wall to improve the aesthetic appearance of the donor site. Prophylactic
anticoagulation with low molecular weight heparin, compression devices, and early ambulation are
recommended to reduce this risk [1,42] .
4. Scar Management: Proper wound care is essential to promote healing and reduce the risk of infection.
Scar management strategies, including silicone gel sheets and pressure garments, may be used to optimize
aesthetic outcomes.
5. Monitoring for Donor-Site Morbidity: Postoperatively, during the immediate and long-term follow-up
period, the donor site should be monitored for complications including abdominal weakness, bulge, or
hernia [43,44] . Regular follow-up is necessary to assess abdominal wall integrity and function.
6. Long-Term Surveillance: Long-term follow-up is necessary to monitor for complications such as fat
necrosis, flap volume changes, and asymmetry.
7. Patient Education and Support: Educating patients about the expected recovery process, potential
complications, and lifestyle modifications is crucial. Providing psychological support and resources for body
image adjustment is also an important aspect of postoperative care.
8. Adjunct Procedures: Secondary procedures, such as autologous fat grafting with donor site contouring or
[45]
nipple-areolar complex reconstruction, may be required to optimize the aesthetic result . These should be
planned based on the individual patient’s needs and desires.