Page 10 - Read Online
P. 10
Fearon et al. Metab Target Organ Damage 2022;2:13 https://dx.doi.org/10.20517/mtod.2022.12 Page 5 of 13
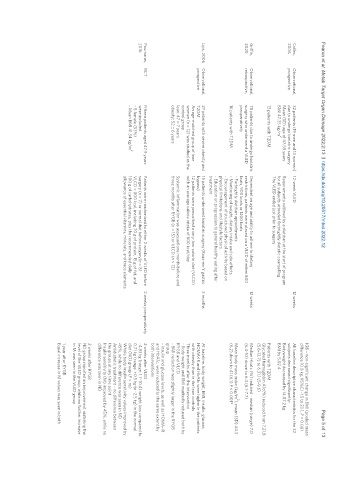
IGB – non-significant change in BMI (pooled mean
difference 10.8 kg, 95%CI -1.5 to 23.1, P = 0.08)
Colles, Observational, 32 patients (19 men and 13 women) 12-week VLED 12 weeks All baseline descriptive characteristics for the 32
2006 prospective due to undergo bariatric surgery subjects decreased significantly:
Mean (SD) age of 47.58 years Requirements outlined by a dietitian at the start of program Bodyweight decreased by 14.87.2 kg
BMI 47.35 kg/m 2 for all subjects attended fortnightly dietetic counselling BMI by 5.02.4
The VLED ended just prior to surgery
13 patients with T2DM Patients with T2DM
Glycated hemoglobin A1c(%) reduced from 7.21.8
(5.6-12.7) to 6.31.1 (5-9.6)
Griffin, Observational, 78 patients due to undergo bariatric Dependent on age and ability to adhere to dietary 12 weeks Median Hba1c (%) reduced - median (range) 7.0
2020 retrospective, surgery who underwent a VLED restrictions, patients were placed on a VLED of either 800 (6.4-10) down to 6.4 (6.1-7.7)
preoperatively kcals, 900 kcals or 1200 kcals
2
- Fortnightly dietitian appointments Mean body mass index (kg/m ), mean (SD) 44.3
16 patients with T2DM - Monitoring of weight, dietary intake and side effects (6.2) down to 41 (6.1) P < 0.001*
- Encouragement of structured physical activity based on
physical limitations and lifestyle factors
- Education on progression to general healthy eating after
treatment
Lips, 2006 Observational, 27 patients with severe obesity and 15 patients underwent bariatric surgery (Roux-en-Y gastric 3 months At baseline, body weight, BMI, insulin, glucose,
prospective T2DM bypass) HOMA-IR and HbA1c were higher in the patients
An age-matched group of lean 12 patients were prescribed a very-low-calorie diet (VLCD) with obesity than in the lean controls
women (n = 12) was studied as the with an average calorie intake of 600 kcal/day Three months after the intervention
control group - Body weight and BMI markedly reduced both by
lean: 47 ± 7 years Systemic inflammation was assessed one month before and RYGB and VLCD
obesity: 52 ± 6 years three months after RYGB (n = 15) or VLCD (n = 12) - BMI reduction was slightly larger in the RYGB
group
- Insulin and glucose levels, as well as HOMA-IR
and HbA1c, were reduced to the same extent by
both interventions
Pournaras, RCT Fifteen patients aged 47.9 years Patients were randomized to either 2 weeks of VLED before 2 weeks preoperatively 2 weeks after VLED
2016 were included surgery (n = 7) or normal diet before surgery(n = 8) -4.83 kg (range: 1.7-10.4) weight loss compared to
- 8 female (53%) VLCD = 800 kcal, including 70 g of protein, 15 g of fat, and 0.71 kg (range: +0.5 kg to -2.5 kg) in the normal
2
- Mean BMI 41.34 kg/m 100 g of carbohydrates, plus the recommended daily diet (ND) group (P = ns)
allowance of essential vitamins, minerals, and trace elements Whole body insulin sensitivity values improved by
45%, while no difference was seen in ND
Antidiabetic treatment - no difference between
the groups at any time point
Insulin sensitivity (M) improved by 45%, while no
difference was seen in ND
2 weeks after RYGB
ND group reported an improvement matching the
level of the VLED group, while no further increase
in M was seen in the VLED group
1 year after RYGB
Equal increase in M values was seen in both