Page 58 - Read Online
P. 58
Latorre-Rodríguez et al. Mini-invasive Surg 2023;7:6 https://dx.doi.org/10.20517/2574-1225.2022.104 Page 7 of 10
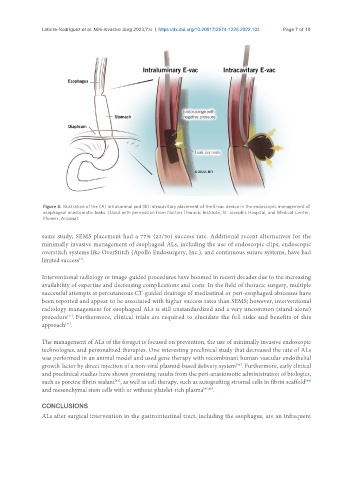
Figure 3. Illustration of the (A) intraluminal and (B) intracavitary placement of the E-vac device in the endoscopic management of
esophageal anastomotic leaks. (Used with permission from Norton Thoracic Institute, St. Joseph’s Hospital, and Medical Center,
Phoenix, Arizona).
same study, SEMS placement had a 77% (23/30) success rate. Additional recent alternatives for the
minimally invasive management of esophageal ALs, including the use of endoscopic clips, endoscopic
overstitch systems like OverStitch (Apollo Endosurgery, Inc.), and continuous suture systems, have had
limited success .
[4]
Interventional radiology or image-guided procedures have boomed in recent decades due to the increasing
availability of expertise and decreasing complications and costs. In the field of thoracic surgery, multiple
successful attempts at percutaneous CT-guided drainage of mediastinal or peri-esophageal abscesses have
been reported and appear to be associated with higher success rates than SEMS; however, interventional
radiology management for esophageal ALs is still unstandardized and a very uncommon (stand-alone)
[41]
procedure . Furthermore, clinical trials are required to elucidate the full risks and benefits of this
approach .
[41]
The management of ALs of the foregut is focused on prevention, the use of minimally invasive endoscopic
technologies, and personalized therapies. One interesting preclinical study that decreased the rate of ALs
was performed in an animal model and used gene therapy with recombinant human vascular endothelial
growth factor by direct injection of a non-viral plasmid-based delivery system . Furthermore, early clinical
[42]
and preclinical studies have shown promising results from the peri-anastomotic administration of biologics,
such as porcine fibrin sealant , as well as cell therapy, such as autografting stromal cells in fibrin scaffold
[44]
[43]
and mesenchymal stem cells with or without platelet-rich plasma [45,46] .
CONCLUSIONS
ALs after surgical intervention in the gastrointestinal tract, including the esophagus, are an infrequent