Page 57 - Read Online
P. 57
Page 6 of 10 Latorre-Rodríguez et al. Mini-invasive Surg 2023;7:6 https://dx.doi.org/10.20517/2574-1225.2022.104
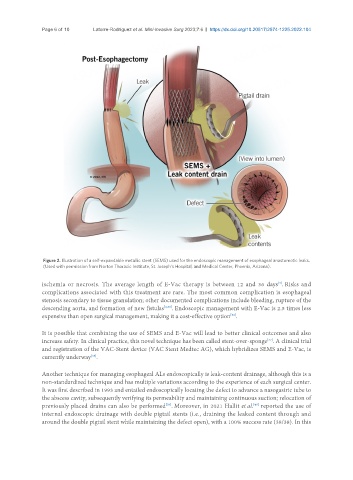
Figure 2. Illustration of a self-expandable metallic stent (SEMS) used for the endoscopic management of esophageal anastomotic leaks.
(Used with permission from Norton Thoracic Institute, St. Joseph’s Hospital, and Medical Center, Phoenix, Arizona).
[4]
ischemia or necrosis. The average length of E-Vac therapy is between 12 and 36 days . Risks and
complications associated with this treatment are rare. The most common complication is esophageal
stenosis secondary to tissue granulation; other documented complications include bleeding, rupture of the
descending aorta, and formation of new fistulas [4,30] . Endoscopic management with E-Vac is 2.5 times less
expensive than open surgical management, making it a cost-effective option .
[36]
It is possible that combining the use of SEMS and E-Vac will lead to better clinical outcomes and also
[37]
increase safety. In clinical practice, this novel technique has been called stent-over-sponge . A clinical trial
and registration of the VAC-Stent device (VAC Stent Medtec AG), which hybridizes SEMS and E-Vac, is
currently underway .
[38]
Another technique for managing esophageal ALs endoscopically is leak-content drainage, although this is a
non-standardized technique and has multiple variations according to the experience of each surgical center.
It was first described in 1993 and entailed endoscopically locating the defect to advance a nasogastric tube to
the abscess cavity, subsequently verifying its permeability and maintaining continuous suction; relocation of
[40]
previously placed drains can also be performed . Moreover, in 2021 Hallit et al. reported the use of
[39]
internal endoscopic drainage with double pigtail stents (i.e., draining the leaked content through and
around the double pigtail stent while maintaining the defect open), with a 100% success rate (38/38). In this