Page 51 - Read Online
P. 51
Yoshizaki et al. Mini-invasive Surg 2022;6:17 https://dx.doi.org/10.20517/2574-1225.2021.116 Page 5 of 9
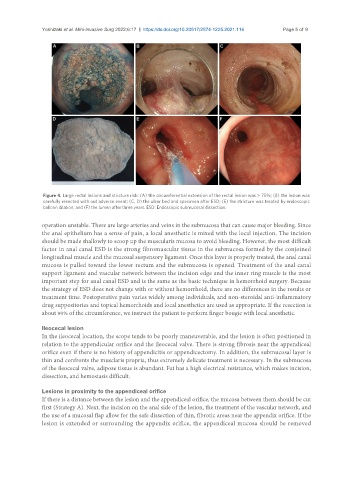
Figure 4. Large rectal lesions and stricture risk: (A) the circumferential extension of the rectal lesion was > 75%; (B) the lesion was
carefully resected with out adverse event; (C, D) the ulcer bed and specimen after ESD; (E) the stricture was treated by endoscopic
balloon dilation; and (F) the lumen after three years. ESD: Endoscopic submucosal dissection.
operation unstable. There are large arteries and veins in the submucosa that can cause major bleeding. Since
the anal epithelium has a sense of pain, a local anesthetic is mixed with the local injection. The incision
should be made shallowly to scoop up the muscularis mucosa to avoid bleeding. However, the most difficult
factor in anal canal ESD is the strong fibromuscular tissue in the submucosa formed by the conjoined
longitudinal muscle and the mucosal suspensory ligament. Once this layer is properly treated, the anal canal
mucosa is pulled toward the lower rectum and the submucosa is opened. Treatment of the anal canal
support ligament and vascular network between the incision edge and the inner ring muscle is the most
important step for anal canal ESD and is the same as the basic technique in hemorrhoid surgery. Because
the strategy of ESD does not change with or without hemorrhoid, there are no differences in the results or
treatment time. Postoperative pain varies widely among individuals, and non-steroidal anti-inflammatory
drug suppositories and topical hemorrhoids and local anesthetics are used as appropriate. If the resection is
about 90% of the circumference, we instruct the patient to perform finger bougie with local anesthetic.
Ileocecal lesion
In the ileocecal location, the scope tends to be poorly maneuverable, and the lesion is often positioned in
relation to the appendicular orifice and the ileocecal valve. There is strong fibrosis near the appendiceal
orifice even if there is no history of appendicitis or appendicectomy. In addition, the submucosal layer is
thin and confronts the musclaris propria, thus extremely delicate treatment is necessary. In the submucosa
of the ileocecal valve, adipose tissue is abundant. Fat has a high electrical resistance, which makes incision,
dissection, and hemostasis difficult.
Lesions in proximity to the appendiceal orifice
If there is a distance between the lesion and the appendiceal orifice, the mucosa between them should be cut
first (Strategy A). Next, the incision on the anal side of the lesion, the treatment of the vascular network, and
the use of a mucosal flap allow for the safe dissection of thin, fibrotic areas near the appendix orifice. If the
lesion is extended or surrounding the appendix orifice, the appendiceal mucosa should be removed