Page 107 - Read Online
P. 107
Cicione et al. Mini-invasive Surg 2021;5:47 https://dx.doi.org/10.20517/2574-1225.2021.52 Page 3 of 11
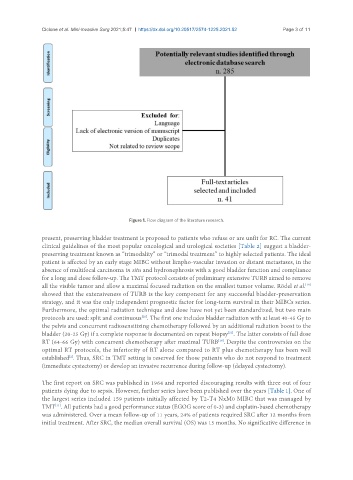
Figure 1. Flow diagram of the literature research.
present, preserving bladder treatment is proposed to patients who refuse or are unfit for RC. The current
clinical guidelines of the most popular oncological and urological societies [Table 2] suggest a bladder-
preserving treatment known as “trimodality” or “trimodal treatment” to highly selected patients. The ideal
patient is affected by an early stage MIBC without limpho-vascular invasion or distant metastases, in the
absence of multifocal carcinoma in situ and hydronephrosis with a good bladder function and compliance
for a long and close follow-up. The TMT protocol consists of preliminary extensive TURB aimed to remove
[19]
all the visible tumor and allow a maximal focused radiation on the smallest tumor volume. Rödel et al.
showed that the extensiveness of TURB is the key component for any successful bladder-preservation
strategy, and it was the only independent prognostic factor for long-term survival in their MIBCs series.
Furthermore, the optimal radiation technique and dose have not yet been standardized, but two main
[20]
protocols are used: split and continuous . The first one includes bladder radiation with at least 40-45 Gy to
the pelvis and concurrent radiosensitizing chemotherapy followed by an additional radiation boost to the
[21]
bladder (20-25 Gy) if a complete response is documented on repeat biopsy . The latter consists of full dose
RT (64-66 Gy) with concurrent chemotherapy after maximal TURB . Despite the controversies on the
[19]
optimal RT protocols, the inferiority of RT alone compared to RT plus chemotherapy has been well
[2]
established . Thus, SRC in TMT setting is reserved for those patients who do not respond to treatment
(immediate cystectomy) or develop an invasive recurrence during follow-up (delayed cystectomy).
The first report on SRC was published in 1964 and reported discouraging results with three out of four
patients dying due to sepsis. However, further series have been published over the years [Table 1]. One of
the largest series included 159 patients initially affected by T2-T4 NxM0 MIBC that was managed by
TMT . All patients had a good performance status (EGOG score of 0-3) and cisplatin-based chemotherapy
[11]
was administered. Over a mean follow-up of 11 years, 24% of patients required SRC after 12 months from
initial treatment. After SRC, the median overall survival (OS) was 15 months. No significative difference in