Page 8 - Read Online
P. 8
Ielpo. Mini-invasive Surg 2021;5:10 I http://dx.doi.org/10.20517/2574-1225.2020.01 Page 3 of 6
A B
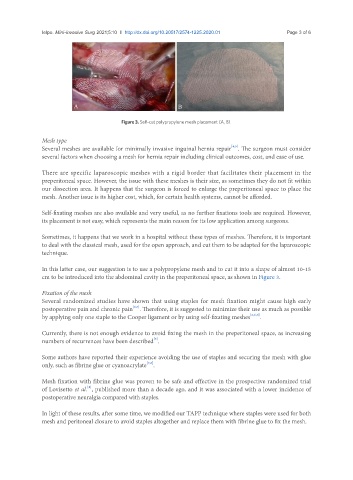
Figure 3. Self-cut polypropylene mesh placement (A, B).
Mesh type
[4,5]
Several meshes are available for minimally invasive inguinal hernia repair . The surgeon must consider
several factors when choosing a mesh for hernia repair including clinical outcomes, cost, and ease of use.
There are specific laparoscopic meshes with a rigid border that facilitates their placement in the
preperitoneal space. However, the issue with these meshes is their size, as sometimes they do not fit within
our dissection area. It happens that the surgeon is forced to enlarge the preperitoneal space to place the
mesh. Another issue is its higher cost, which, for certain health systems, cannot be afforded.
Self-fixating meshes are also available and very useful, as no further fixations tools are required. However,
its placement is not easy, which represents the main reason for its low application among surgeons.
Sometimes, it happens that we work in a hospital without these types of meshes. Therefore, it is important
to deal with the classical mesh, used for the open approach, and cut them to be adapted for the laparoscopic
technique.
In this latter case, our suggestion is to use a polypropylene mesh and to cut it into a shape of almost 10-15
cm to be introduced into the abdominal cavity in the preperitoneal space, as shown in Figure 3.
Fixation of the mesh
Several randomized studies have shown that using staples for mesh fixation might cause high early
[6,7]
postoperative pain and chronic pain . Therefore, it is suggested to minimize their use as much as possible
by applying only one staple to the Cooper ligament or by using self-fixating meshes [2,6,7] .
Currently, there is not enough evidence to avoid fixing the mesh in the preperitoneal space, as increasing
[3]
numbers of recurrences have been described .
Some authors have reported their experience avoiding the use of staples and securing the mesh with glue
[7,8]
only, such as fibrine glue or cyanoacrylate .
Mesh fixation with fibrine glue was proven to be safe and effective in the prospective randomized trial
[8]
of Lovisetto et al. , published more than a decade ago, and it was associated with a lower incidence of
postoperative neuralgia compared with staples.
In light of these results, after some time, we modified our TAPP technique where staples were used for both
mesh and peritoneal closure to avoid staples altogether and replace them with fibrine glue to fix the mesh.