Page 58 - Read Online
P. 58
Page 6 of 12 Belli et al. Mini-invasive Surg 2020;4:77 I http://dx.doi.org/10.20517/2574-1225.2020.70
#
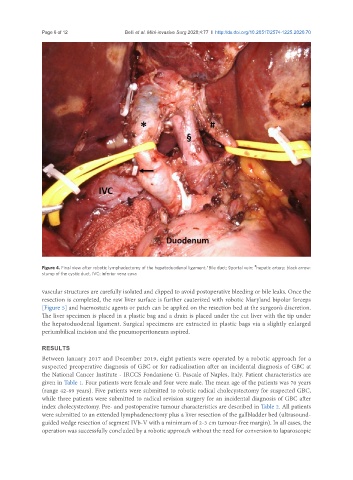
Figure 4. Final view after robotic lymphadectomy of the hepatoduodenal ligament.*Bile duct; §portal vein; hepatic artery; black arrow:
stump of the cystic duct. IVC: inferior vena cava
vascular structures are carefully isolated and clipped to avoid postoperative bleeding or bile leaks. Once the
resection is completed, the raw liver surface is further cauterized with robotic Maryland bipolar forceps
[Figure 5] and haemostatic agents or patch can be applied on the resection bed at the surgeon’s discretion.
The liver specimen is placed in a plastic bag and a drain is placed under the cut liver with the tip under
the hepatoduodenal ligament. Surgical specimens are extracted in plastic bags via a slightly enlarged
periumbilical incision and the pneumoperitoneum aspired.
RESULTS
Between January 2017 and December 2019, eight patients were operated by a robotic approach for a
suspected preoperative diagnosis of GBC or for radicalisation after an incidental diagnosis of GBC at
the National Cancer Institute - IRCCS Fondazione G. Pascale of Naples, Italy. Patient characteristics are
given in Table 1. Four patients were female and four were male. The mean age of the patients was 70 years
(range 42-89 years). Five patients were submitted to robotic radical cholecystectomy for suspected GBC,
while three patients were submitted to radical revision surgery for an incidental diagnosis of GBC after
index cholecystectomy. Pre- and postoperative tumour characteristics are described in Table 2. All patients
were submitted to an extended lymphadenectomy plus a liver resection of the gallbladder bed (ultrasound-
guided wedge resection of segment IVb-V with a minimum of 2-3 cm tumour-free margin). In all cases, the
operation was successfully concluded by a robotic approach without the need for conversion to laparoscopic