Page 47 - Read Online
P. 47
Page 2 of 8 Golhar et al. Mini-invasive Surg 2019;3:9 I http://dx.doi.org/10.20517/2574-1225.2018.58
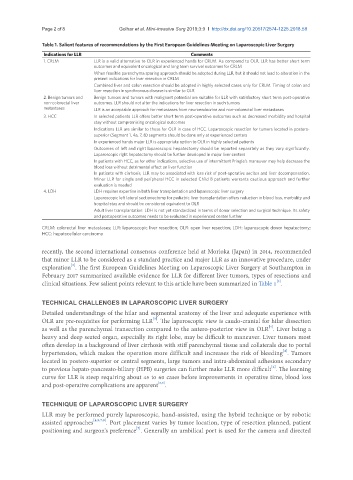
Table 1. Salient features of recommendations by the First European Guidelines Meeting on Laparoscopic Liver Surgery
Indications for LLR Comments
1. CRLM LLR is a valid alternative to OLR in experienced hands for CRLM. As compared to OLR, LLR has better short term
outcomes and equivalent oncological and long term survival outcomes for CRLM
When feasible parenchyma sparing approach should be adopted during LLR, but it should not lead to alteration in the
present indications for liver resection in CRLM
Combined liver and colon resection should be adopted in highly selected cases only for CRLM. Timing of colon and
liver resection in synchronous disease is similar to OLR
2. Benign tumors and Benign tumors and tumors with malignant potential are suitable for LLR with satisfactory short term post-operative
non-colorectal liver outcomes. LLR should not alter the indications for liver resection in such tumors
metastases LLR is an acceptable approach for metastases from neuroendocrine and non-colorectal liver metastases
3. HCC In selected patients LLR offers better short term post-operative outcomes such as decreased morbidity and hospital
stay without compromising oncological outcomes
Indications LLR are similar to those for OLR in case of HCC. Laparoscopic resection for tumors located in postero-
superior (Segment 1, 4a, 7, 8) segments should be done only at experienced centers
In experienced hands major LLR is appropriate option to OLR in highly selected patients
Outcomes of left and right laparoscopic hepatectomy should be reported separately as they vary significantly.
Laparoscopic right hepatectomy should be further developed in major liver centers
In patients with HCC, as for other indications, selective use of intermittent Pringle’s maneuver may help decrease the
blood loss without detrimental effect on liver function
In patients with cirrhosis, LLR may be associated with less risk of post-operative ascites and liver decompensation.
Minor LLR for single and peripheral HCC in selected Child B patients warrants cautious approach and further
evaluation is needed
4. LDH LDH requires expertise in both liver transplantation and laparoscopic liver surgery
Laparoscopic left lateral sectionectomy for pediatric liver transplantation offers reduction in blood loss, morbidity and
hospital stay and should be considered equivalent to OLR
Adult liver transplantation: LDH is not yet standardized in terms of donor selection and surgical technique. Its safety
and postoperative outcomes needs to be evaluated in experienced center further
CRLM: colorectal liver metastases; LLR: laparoscopic liver resection; OLR: open liver resection; LDH: laparoscopic donor hepatectomy;
HCC: hepatocellular carcinoma
recently, the second international consensus conference held at Morioka (Japan) in 2014, recommended
that minor LLR to be considered as a standard practice and major LLR as an innovative procedure, under
[2]
exploration . The first European Guidelines Meeting on Laparoscopic Liver Surgery at Southampton in
February 2017 summarized available evidence for LLR for different liver tumors, types of resections and
[3]
clinical situations. Few salient points relevant to this article have been summarized in Table 1 .
TECHNICAL CHALLENGES IN LAPAROSCOPIC LIVER SURGERY
Detailed understandings of the hilar and segmental anatomy of the liver and adequate experience with
[3]
OLR are pre-requisites for performing LLR . The laparoscopic view is caudo-cranial for hilar dissection
[4]
as well as the parenchymal transection compared to the antero-posterior view in OLR . Liver being a
heavy and deep seated organ, especially its right lobe, may be difficult to maneuver. Liver tumors most
often develop in a background of liver cirrhosis with stiff parenchymal tissue and collaterals due to portal
[4]
hypertension, which makes the operation more difficult and increases the risk of bleeding . Tumors
located in postero-superior or central segments, large tumors and intra-abdominal adhesions secondary
[4]
to previous hepato-pancreato-biliary (HPB) surgeries can further make LLR more difficult . The learning
curve for LLR is steep requiring about 45 to 60 cases before improvements in operative time, blood loss
[5,6]
and post-operative complications are apparent .
TECHNIQUE OF LAPAROSCOPIC LIVER SURGERY
LLR may be performed purely laparoscopic, hand-assisted, using the hybrid technique or by robotic
assisted approaches [4,5,7,8] . Port placement varies by tumor location, type of resection planned, patient
[7]
positioning and surgeon’s preference . Generally an umbilical port is used for the camera and directed