Page 69 - Read Online
P. 69
Rosales et al. J Transl Genet Genom 2020;4:81-90 I https://doi.org/10.20517/jtgg.2020.12 Page 87
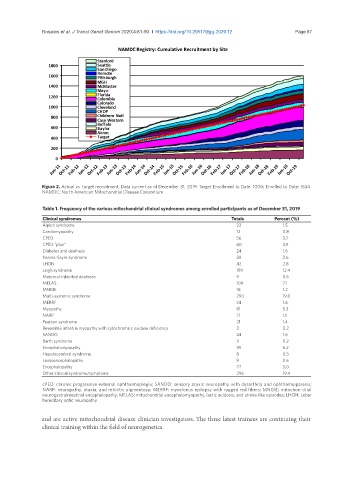
Figure 2. Actual vs. target recruitment. Data current as of December 31, 2019. Target Enrollment to Date: 1000; Enrolled to Date: 1634.
NAMDC: North American Mitochondrial Disease Consortium
Table 1. Frequency of the various mitochondrial clinical syndromes among enrolled participants as of December 31, 2019
Clinical syndromes Totals Percent (%)
Alpers syndrome 23 1.5
Cardiomyopathy 12 0.8
CPEO 56 3.7
CPEO “plus” 60 3.9
Diabetes and deafness 24 1.6
Kearns-Sayre syndrome 39 2.6
LHON 42 2.8
Leigh syndrome 189 12.4
Maternal-inherited deafness 9 0.6
MELAS 109 7.1
MNGIE 18 1.2
Multi-systemic syndrome 290 19.0
MERRF 24 1.6
Myopathy 81 5.3
NARP 17 1.1
Pearson syndrome 21 1.4
Reversible infantile myopathy with cytochrome c oxidase deficiency 3 0.2
SANDO 24 1.6
Barth syndrome 3 0.2
Encephalomyopathy 95 6.2
Hepatocerebral syndrome 8 0.5
Leukoencephalopathy 9 0.6
Encephalopathy 77 5.0
Other clinical syndrome/symptoms 296 19.4
cPEO: chronic progressive external ophthalmoplegia; SANDO: sensory ataxic neuropathy with dysarthria and ophthalmoparesis;
NARP: neuropathy, ataxia, and retinitis pigmentosa; MERRF: myoclonus epilepsy with ragged red fibers; MNGIE: mitochon-drial
neurogastrointestinal encephalopathy; MELAS: mitochondrial encephalomyopathy, lactic acidosis, and stroke-like episodes; LHON: Leber
hereditary optic neuropathy
and are active mitochondrial disease clinician investigators. The three latest trainees are continuing their
clinical training within the field of neurogenetics.