Page 58 - Read Online
P. 58
Page 26 of 33 Berardi et al. J Cancer Metastasis Treat 2019;5:79 I http://dx.doi.org/10.20517/2394-4722.2019.008
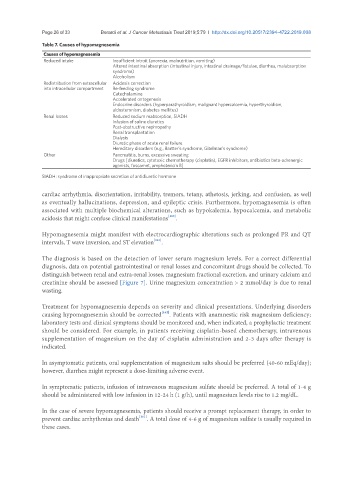
Table 7. Causes of hypomagnesemia
Causes of hypomagnesemia
Reduced intake Insufficient introit (anorexia, malnutrition, vomiting)
Altered intestinal absorption (intestinal injury, intestinal drainage/fistulae, diarrhea, malabsorption
syndrome)
Alcoholism
Redistribution from extracellular Acidosis correction
into intracellular compartment Re-feeding syndrome
Catecholamine
Accelerated ontogenesis
Endocrine disorders (hyperparathyroidism, malignant hypercalcemia, hyperthyroidism,
aldosteronism, diabetes mellitus)
Renal losses Reduced sodium reabsorption, SIADH
Infusion of saline diuretics
Post-obstructive nephropathy
Renal transplantation
Dialysis
Diuretic phase of acute renal failure
Hereditary disorders (e.g., Bartter’s syndrome, Gitelman’s syndrome)
Other Pancreatitis, burns, excessive sweating
Drugs [diuretics, cytotoxic chemotherapy (cisplatin), EGFR inhibitors, antibiotics beta-adrenergic
agonists, foscarnet, amphotericin B]
SIADH: syndrome of inappropriate secretion of antidiuretic hormone
cardiac arrhythmia, disorientation, irritability, tremors, tetany, athetosis, jerking, and confusion, as well
as eventually hallucinations, depression, and epileptic crisis. Furthermore, hypomagnesemia is often
associated with multiple biochemical alterations, such as hypokalemia, hypocalcemia, and metabolic
acidosis that might confuse clinical manifestations [160] .
Hypomagnesemia might manifest with electrocardiographic alterations such as prolonged PR and QT
intervals, T wave inversion, and ST elevation [161] .
The diagnosis is based on the detection of lower serum magnesium levels. For a correct differential
diagnosis, data on potential gastrointestinal or renal losses and concomitant drugs should be collected. To
distinguish between renal and extra-renal losses, magnesium fractional excretion, and urinary calcium and
creatinine should be assessed [Figure 7]. Urine magnesium concentration > 2 mmol/day is due to renal
wasting.
Treatment for hypomagnesemia depends on severity and clinical presentations. Underlying disorders
causing hypomagnesemia should be corrected [162] . Patients with anamnestic risk magnesium deficiency;
laboratory tests and clinical symptoms should be monitored and, when indicated, a prophylactic treatment
should be considered. For example, in patients receiving cisplatin-based chemotherapy, intravenous
supplementation of magnesium on the day of cisplatin administration and 2-3 days after therapy is
indicated.
In asymptomatic patients, oral supplementation of magnesium salts should be preferred (40-60 mEq/day);
however, diarrhea might represent a dose-limiting adverse event.
In symptomatic patients, infusion of intravenous magnesium sulfate should be preferred. A total of 1-4 g
should be administered with low infusion in 12-24 h (1 g/h), until magnesium levels rise to 1.2 mg/dL.
In the case of severe hypomagnesemia, patients should receive a prompt replacement therapy, in order to
prevent cardiac arrhythmias and death [161] . A total dose of 4-6 g of magnesium sulfate is usually required in
these cases.