Page 23 - Read Online
P. 23
Matsuoka et al. J Cancer Metastasis Treat 2018;4:6 I http://dx.doi.org/10.20517/2394-4722.2017.85 Page 9 of 13
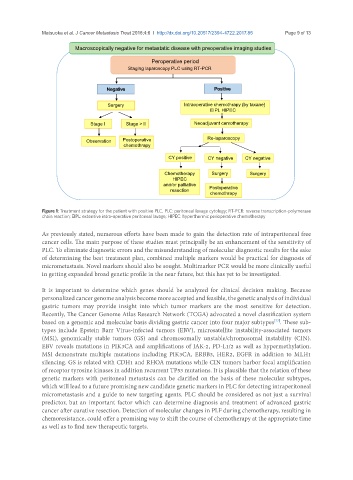
Macroscopically negative for metastatic disease with preoperative imaging studies
Peroperative period
Staging laparoscopy PLC using RT-PCR
Negative Positive
Surgery Intraoperative chemothrapy (by taxane)
EIPL HIPEC
Stage I Stage > II Neoadjuvant cemotherapy
Observation Postoperative Re-laparoscopy
chemothrapy
CY positive CY negative CY negative
Chemotherapy Surgery Surgery
HIPEC
and/or palliative
resection Postoperative
chemothrapy
EIPL: Extensive intra-operative peritoneal lavage. HIPEC : hyperthermic perioperative chemotherapy
Figure 1: Treatment strategy for the patient with positive PLC. PLC: peritoneal lavage cytology; RT-PCR: reverse transcription-polymerase
Figure. Treatment strategy for the patient with positive PLC
chain reaction; EIPL: extensive intra-operative peritoneal lavage; HIPEC: hyperthermic perioperative chemotherapy
As previously stated, numerous efforts have been made to gain the detection rate of intraperitoneal free
cancer cells. The main purpose of these studies must principally be an enhancement of the sensitivity of
PLC. To eliminate diagnostic errors and the misunderstanding of molecular diagnostic results for the sake
of determining the best treatment plan, combined multiple markers would be practical for diagnosis of
micrometastasis. Novel markers should also be sought. Multimarker PCR would be more clinically useful
in getting expanded broad genetic profile in the near future, but this has yet to be investigated.
It is important to determine which genes should be analyzed for clinical decision making. Because
personalized cancer genome analysis become more accepted and feasible, the genetic analysis of individual
gastric tumors may provide insight into which tumor markers are the most sensitive for detection.
Recently, The Cancer Genome Atlas Research Network (TCGA) advocated a novel classification system
based on a genomic and molecular basis dividing gastric cancer into four major subtypes . These sub-
[77]
types include Epstein Barr Virus-infected tumors (EBV), microsatellite instability-associated tumors
(MSI), genomically stable tumors (GS) and chromosomally unstable/chromosomal instability (CIN).
EBV reveals mutations in PIK3CA and amplifications of JAK-2, PD-L1/2 as well as hypermethylation.
MSI demonstrate multiple mutations including PIK3CA, ERBB3, HER2, EGFR in addition to MLH1
silencing. GS is related with CDH1 and RHOA mutations while CIN tumors harbor focal amplification
of receptor tyrosine kinases in addition recurrent TP53 mutations. It is plausible that the relation of these
genetic markers with peritoneal metastasis can be clarified on the basis of these molecular subtypes,
which will lead to a future promising new candidate genetic markers in PLC for detecting intraperitoneal
micrometastasis and a guide to new targeting agents. PLC should be considered as not just a survival
predictor, but an important factor which can determine diagnosis and treatment of advanced gastric
cancer after curative resection. Detection of molecular changes in PLF during chemotherapy, resulting in
chemoresistance, could offer a promising way to shift the course of chemotherapy at the appropriate time
as well as to find new therapeutic targets.