Page 56 - Read Online
P. 56
Chan et al. Hepatoma Res 2018;4:5 I http://dx.doi.org/10.20517/2394-5079.2017.49 Page 5 of 17
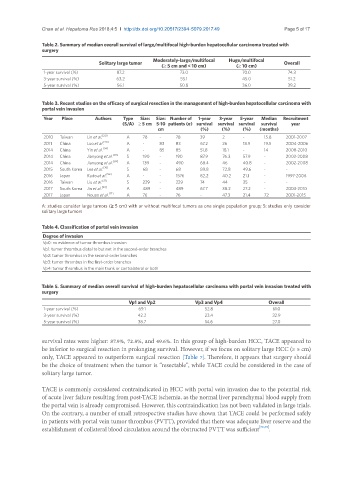
Table 2. Summary of median overall survival of large/multifocal high-burden hepatocellular carcinoma treated with
surgery
Moderately-large/multifocal Huge/multifocal
Solitary large tumor Overall
(≥ 5 cm and < 10 cm) (≥ 10 cm)
1-year survival (%) 87.2 73.0 70.0 74.3
3-year survival (%) 63.2 55.1 45.0 51.2
5-year survival (%) 56.1 50.8 36.0 39.2
Table 3. Recent studies on the efficacy of surgical resection in the management of high-burden hepatocellular carcinoma with
portal vein invasion
Year Place Authors Type Size: Size: Number of 1-year 3-year 5-year Median Recruitment
(S/A) ≥ 5 cm 5-10 patients (n) survival survival survival survival year
cm (%) (%) (%) (months)
2010 Taiwan Lin et al. [20] A 78 - 78 39 2 - 15.8 2001-2007
2011 China Luo et al. [26] A - 83 83 67.2 26 18.9 19.5 2004-2006
2014 China Yin et al. [34] A - 85 85 51.8 18.1 - 14 2008-2010
2014 China Jianyong et al. [69] S 190 - 190 87.9 76.3 57.9 - 2002-2008
2014 China Jianyong et al. [69] A 139 - 490 68.4 46 40.8 - 2002-2008
2015 South Korea Lee et al. [70] S 68 - 68 89.8 72.8 49.6 - -
2016 Japan Kudo et al. [56] A - - 1576 82.2 40.2 21.1 - 1997-2006
2016 Taiwan Liu et al. [37] S 229 - 229 74 44 35 - -
2017 South Korea Jin et al. [39] A 489 - 489 67.7 38.2 27.2 - 2003-2010
2017 Japan Nouso et al. [71] A 76 - 76 - 47.3 21.4 72 2001-2015
A: studies consider large tumors (≥ 5 cm) with or without multifocal tumors as one single population group; S: studies only consider
solitary large tumors
Table 4. Classification of portal vein invasion
Degree of invasion
Vp0: no evidence of tumor thrombus invasion
Vp1: tumor thrombus distal to but not in the second-order branches
Vp2: tumor thrombus in the second-order branches
Vp3: tumor thrombus in the first-order branches
Vp4: tumor thrombus in the main trunk or contralateral or both
Table 5. Summary of median overall survival of high-burden hepatocellular carcinoma with portal vein invasion treated with
surgery
Vp1 and Vp2 Vp3 and Vp4 Overall
1-year survival (%) 69.1 52.8 61.0
3-year survival (%) 42.2 23.4 32.9
5-year survival (%) 38.7 14.6 27.0
survival rates were higher: 87.9%, 72.8%, and 49.6%. In this group of high-burden HCC, TACE appeared to
be inferior to surgical resection in prolonging survival. However, if we focus on solitary large HCC (≥ 5 cm)
only, TACE appeared to outperform surgical resection [Table 7]. Therefore, it appears that surgery should
be the choice of treatment when the tumor is “resectable”, while TACE could be considered in the case of
solitary large tumor.
TACE is commonly considered contraindicated in HCC with portal vein invasion due to the potential risk
of acute liver failure resulting from post-TACE ischemia, as the normal liver parenchymal blood supply from
the portal vein is already compromised. However, this contraindication has not been validated in large trials.
On the contrary, a number of small retrospective studies have shown that TACE could be performed safely
in patients with portal vein tumor thrombus (PVTT), provided that there was adequate liver reserve and the
establishment of collateral blood circulation around the obstructed PVTT was sufficient [72,73] .