Page 44 - Read Online
P. 44
Robichaux et al. LLR in the cirrhotic patient
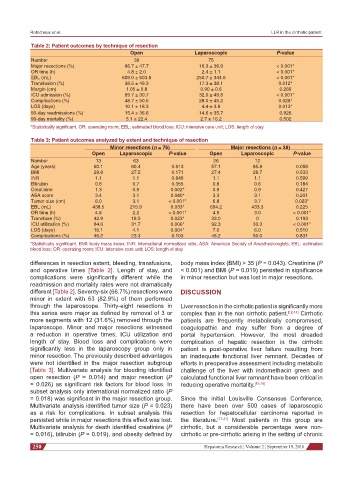
Table 2: Patient outcomes by technique of resection
Open Laparoscopic P-value
Number 39 75
Major resections (%) 66.7 ± 47.7 16.3 ± 36.9 < 0.001*
OR time (h) 4.8 ± 2.0 2.4 ± 1.1 < 0.001*
EBL (mL) 609.0 ± 603.8 250.7 ± 344.6 < 0.001*
Transfusion (%) 38.5 ± 49.3 17.3 ± 38.1 0.012*
Margin (cm) 1.05 ± 0.8 0.90 ± 0.6 0.269
ICU admission (%) 89.7 ± 30.7 32.0 ± 49.8 < 0.001*
Complications (%) 48.7 ± 50.5 28.0 ± 45.2 0.028*
LOS (days) 10.1 ± 18.3 4.4 ± 3.8 0.013*
90-day readmissions (%) 15.4 ± 36.6 14.6 ± 35.7 0.926
90-day mortality (%) 5.1 ± 22.4 2.7 ± 16.2 0.502
*Statistically significant. OR: operating room; EBL: estimated blood loss; ICU: intensive care unit; LOS: length of stay
Table 3: Patient outcomes analyzed by extent and technique of resection
Minor resections (n = 76) Major resections (n = 38)
Open Laparoscopic P-value Open Laparoscopic P-value
Number 13 63 26 12
Age (years) 60.1 60.4 0.913 57.1 65.8 0.058
BMI 29.8 27.5 0.171 27.4 28.7 0.533
INR 1.1 1.1 0.846 1.1 1.1 0.599
Bilirubin 0.8 0.7 0.355 0.8 0.6 0.184
Creatinine 1.3 0.9 0.002* 0.9 0.9 0.427
ASA score 3.4 3.1 0.040* 3.3 3.1 0.201
Tumor size (cm) 6.0 3.1 < 0.001* 6.8 3.7 0.023*
EBL (mL) 438.5 215.9 0.033* 694.2 433.3 0.225
OR time (h) 4.8 2.2 < 0.001* 4.9 3.0 < 0.001*
Transfuse (%) 42.9 18.5 0.023* 33.0 0 0.193
ICU utilization (%) 84.6 31.7 0.006* 92.3 33.3 < 0.001*
LOS (days) 16.1 4.1 0.004* 7.0 6.0 0.510
Complications (%) 46.2 23.3 0.103 46.2 50.0 0.831
*Statistically significant. BMI: body mass index; INR: international normalized ratio; ASA: American Society of Anesthesiologists; EBL: estimated
blood loss; OR: operating room; ICU: intensive care unit; LOS: length of stay
differences in resection extent, bleeding, transfusions, body mass index (BMI) > 35 (P = 0.043). Creatinine (P
and operative times [Table 2]. Length of stay, and < 0.001) and BMI (P = 0.019) persisted in significance
complications were significantly different while the in minor resection but was lost in major resections.
readmission and mortality rates were not dramatically
different [Table 2]. Seventy-six (66.7%) resections were DISCUSSION
minor in extent with 63 (82.9%) of them performed
through the laparoscope. Thirty-eight resections in Liver resection in the cirrhotic patient is significantly more
this series were major as defined by removal of 3 or complex than in the non cirrhotic patient. [12-14] Cirrhotic
more segments with 12 (31.6%) removed through the patients are frequently metabolically compromised,
laparoscope. Minor and major resections witnessed coagulopathic and may suffer from a degree of
a reduction in operative times, ICU utilization and portal hypertension. However, the most dreaded
length of stay. Blood loss and complications were complication of hepatic resection in the cirrhotic
significantly less in the laparoscopy group only in patient is post-operative liver failure resulting from
minor resection. The previously described advantages an inadequate functional liver remnant. Decades of
were not identified in the major resection subgroup efforts in preoperative assessment including metabolic
[Table 3]. Multivariate analysis for bleeding identified challenge of the liver with indomethacin green and
open resection (P = 0.014) and major resection (P calculated functional liver remnant have been critical in
= 0.026) as significant risk factors for blood loss. In reducing operative mortality. [15,16]
subset analysis only international normalized ratio (P
= 0.018) was significant in the major resection group. Since the initial Louisville Consensus Conference,
Multivariate analysis identified tumor size (P = 0.023) there have been over 500 cases of laparoscopic
as a risk for complications. In subset analysis this resection for hepatocellular carcinoma reported in
persisted while in major resections this effect was lost. the literature. [17-21] Most patients in this group are
Multivariate analysis for death identified creatinine (P cirrhotic, but a considerable percentage were non-
= 0.016), bilirubin (P = 0.019), and obesity defined by cirrhotic or pre-cirrhotic arising in the setting of chronic
250 Hepatoma Research ¦ Volume 2 ¦ September 19, 2016