Page 38 - Read Online
P. 38
Kilburn et al. Laparoscopic resection of HCC
Table 3: Postoperative and histopathological data
Postoperative and All patients Non-cirrhotic Cirrhotic
histopathological data
Length of hospital stay, days, 5 (1-72) 5 (3-13) 5 (1-72)
median (range)
Mortality, 90-day, n (%) 1 (1.9) 0 (0) 1 (3)
Overall morbidity, n (%) 7 (13) 2 (11) 5 (15)
Infection 3 (6) 1 (6) 2 (6)
Ascites 3 (6) 0 (0) 3 (9)
Bile leak 1 (2) 1 (6) 0 (0)
Tumor margin, mm, median 9 5 15
Margin status, n (%)
R0 48 (92) 17 (94) 31 (91)
R1 4 (8) 1 (6) 3 (9)
Tumor size, mm, median (range) 33 (5-220) 40 (20-150) 28 (5-220)
Number of tumors, median (range) 1 (1-5) 1 (1-2) 1 (1-5)
Multifocality, n (%) 17 (33) 2 (11) 15 (44)
Tumor differentiation, n (%)
Well differentiated 13 (25) 6 (33) 9 (26)
Moderately differentiated 36 (70) 11 (61) 23 (67)
Poorly differentiated 3 (5) 1 (6) 2 (6)
Vascular invasion, n (%) 17 (33) 8 (44) 9 (26)
Lymphatic invasion, n (%) 4 (9) 1 (6) 3 (9)
Subsequent cases involving dome lesions were different between patients with and without cirrhosis.
preferentially performed with a combined transthoracic Apart from the single post-operative mortality, all
and transabdominal approach. complications were Clavien-Dindo grade 1 or 2.
Median operative time was 120 min and median blood Multifocal HCC was far more prevalent in cirrhotics
loss was 300 mL. Patients with cirrhosis experienced compared with non-cirrhotics (44% vs. 11%, P = 0.008).
more bleeding than those without (median 350 mL in Multifocality was generally diagnosed incidentally on
cirrhotics vs. 150 mL in non-cirrhotics, P = 0.049). The pathology of the resected specimen as patients with
median length of stay was 5 days and was not different multifocal disease were excluded from resection.
between the cirrhotic and non-cirrhotic groups. Microvascular invasion was present in 17 patients
(33%). Equivalent R0 resection rates were achieved
Postoperative and pathological data are summarized in for cirrhotics and non-cirrhotics (94% vs. 91%). Despite
Table 3. There was 1 mortality, which occurred early in the higher rate of subsegmental resections, the median
the series. The patient had Child-Pugh B cirrhosis and margin in cirrhotics was 15 mm compared with 5 mm in
underwent a left lateral sectionectomy. Blood loss was the non-cirrhotics (P = 0.067).
1,600 mL and this patient died due to decompensated
liver failure. Overall 7 patients (13%) developed a Median follow-up was 41 months. Median overall
postoperative complication. Morbidity rates were not survival was 89 months. Overall survival for the entire
cohort at 1, 3, and 5 years was 88%, 81%, and 61%,
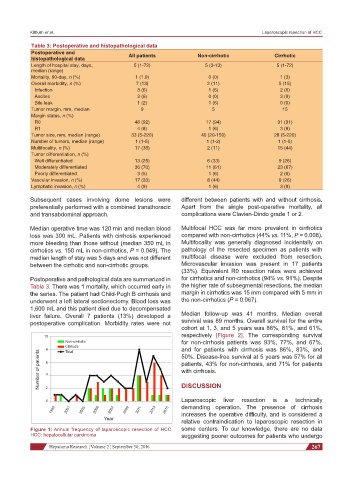
10 respectively [Figure 2]. The corresponding survival
Non-cirrhotic for non-cirrhosis patients was 93%, 77%, and 67%,
Cirrhotic
8 Total and for patients with cirrhosis was 86%, 83%, and
Number of patients 6 4 patients, 43% for non-cirrhosis, and 71% for patients
50%. Disease-free survival at 5 years was 57% for all
with cirrhosis.
DISCUSSION
0 2 Laparoscopic liver resection is a technically
1999 2001 2003 2005 2007 2009 2011 2013 2015 demanding operation. The presence of cirrhosis
increases the operative difficulty, and is considered a
Year
relative contraindication to laparoscopic resection in
Figure 1: Annual frequency of laparoscopic resection of HCC. some centers. To our knowledge, there are no data
HCC: hepatocellular carcinoma suggesting poorer outcomes for patients who undergo
Hepatoma Research ¦ Volume 2 ¦ September 30, 2016 267