Page 31 - Read Online
P. 31
Ratti et al. Fast-track management in patients with HCC
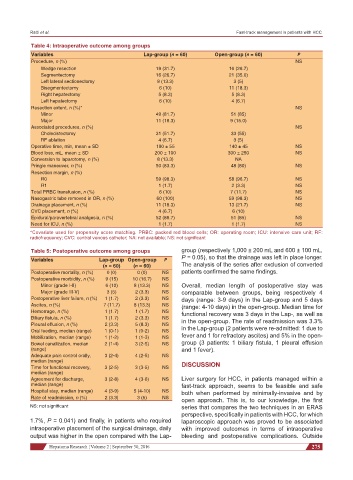
Table 4: Intraoperative outcome among groups
Variables Lap-group (n = 60) Open-group (n = 60) P
Procedure, n (%) NS
Wedge resection 19 (31.7) 16 (26.7)
Segmentectomy 16 (26.7) 21 (35.0)
Left lateral sectionectomy 8 (13.3) 3 (5)
Bisegmentectomy 6 (10) 11 (18.3)
Right hepatectomy 5 (8.3) 5 (8.3)
Left hepatectomy 6 (10) 4 (6.7)
Resection extent, n (%)* NS
Minor 49 (81.7) 51 (85)
Major 11 (18.3) 9 (15.0)
Associated procedures, n (%) NS
Cholecistectomy 31 (51.7) 33 (55)
RF ablation 4 (6.7) 3 (5)
Operative time, min, mean ± SD 190 ± 55 140 ± 45 NS
Blood loss, mL, mean ± SD 200 ± 100 300 ± 250 NS
Conversion to laparotomy, n (%) 8 (13.3) NA
Pringle maneuver, n (%) 50 (83.3) 48 (80) NS
Resection margin, n (%)
R0 59 (98.3) 58 (96.7) NS
R1 1 (1.7) 2 (3.3) NS
Total PRBC transfusion, n (%) 6 (10) 7 (11.7) NS
Nasogastric tube removed in OR, n (%) 60 (100) 59 (98.3) NS
Drainage placement, n (%) 11 (18.3) 13 (21.7) NS
CVC placement, n (%) 4 (6.7) 6 (10)
Epidural/paravertebral analgesia, n (%) 52 (86.7) 51 (85) NS
Need for ICU, n (%) 1 (1.7) 1 (1.7) NS
*Covariate used for propensity score matching. PRBC: packed red blood cells; OR: operating room; ICU: intensive care unit; RF:
radiofrequency; CVC: central venous catheter; NA: not available; NS: not significant
Table 5: Postoperative outcome among groups group (respectively 1,000 ± 200 mL and 600 ± 100 mL,
Variables Lap-group Open-group P P = 0.05), so that the drainage was left in place longer.
(n = 60) (n = 60) The analysis of the series after exclusion of converted
Postoperative mortality, n (%) 0 (0) 0 (0) NS patients confirmed the same findings.
Postoperative morbidity, n (%) 9 (15) 10 (16.7) NS
Minor (grade I-II) 6 (10) 8 (13.3) NS Overall, median length of postoperative stay was
Major (grade III-V) 3 (5) 2 (3.3) NS comparable between groups, being respectively 4
Postoperative liver failure, n (%) 1 (1.7) 2 (3.3) NS days (range: 3-9 days) in the Lap-group and 5 days
Ascites, n (%) 7 (11.7) 8 (13.3) NS (range: 4-10 days) in the open-group. Median time for
Hemorrage, n (%) 1 (1.7) 1 (1.7) NS functional recovery was 3 days in the Lap-, as well as
Biliary fistula, n (%) 1 (1.7) 2 (3.3) NS in the open-group. The rate of readmission was 3.3%
Pleural effusion, n (%) 2 (3.3) 5 (8.3) NS
Oral feeding, median (range) 1 (0-1) 1 (0-2) NS in the Lap-group (2 patients were re-admitted: 1 due to
Mobilization, median (range) 1 (1-2) 1 (1-3) NS fever and 1 for refractory ascites) and 5% in the open-
Bowel canalization, median 2 (1-4) 3 (2-5) NS group (3 patients: 1 biliary fistula, 1 pleural effusion
(range) and 1 fever).
Adequate pain control orally, 3 (2-4) 4 (2-5) NS
median (range) DISCUSSION
Time for functional recovery, 3 (2-5) 3 (3-5) NS
median (range)
Agreement for discharge, 3 (2-8) 4 (3-6) NS Liver surgery for HCC, in patients managed within a
median (range) fast-track approach, seems to be feasible and safe
Hospital stay, median (range) 4 (3-9) 5 (4-10) NS both when performed by minimally-invasive and by
Rate of readmission, n (%) 2 (3.3) 3 (5) NS open approach. This is, to our knowledge, the first
NS: not significant series that compares the two techniques in an ERAS
perspective, specifically in patients with HCC, for which
1.7%, P = 0.041) and finally, in patients who required laparoscopic approach was proved to be associated
intraoperative placement of the surgical drainage, daily with improved outcomes in terms of intraoperative
output was higher in the open compared with the Lap- bleeding and postoperative complications. Outside
Hepatoma Research ¦ Volume 2 ¦ September 30, 2016 275