Page 56 - Read Online
P. 56
Wu et al. Hepatoma Res 2023;9:6 https://dx.doi.org/10.20517/2394-5079.2022.37 Page 3 of 15
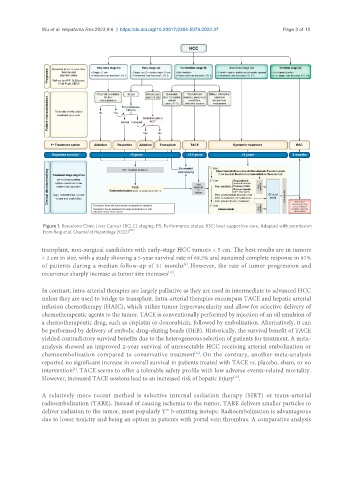
Figure 1. Barcelona Clinic Liver Cancer (BCLC) staging. PS: Performance status; BSC: best supportive care. Adapted with permission
from Reig et al. (Journal of Hepatology 2022) [10] .
transplant, non-surgical candidates with early-stage HCC tumors < 5 cm. The best results are in tumors
< 2 cm in size, with a study showing a 5-year survival rate of 68.5% and sustained complete response in 97%
[3]
of patients during a median follow-up of 31 months . However, the rate of tumor progression and
[15]
recurrence sharply increase as tumor size increases .
In contrast, intra-arterial therapies are largely palliative as they are used in intermediate to advanced HCC
unless they are used to bridge to transplant. Intra-arterial therapies encompass TACE and hepatic arterial
infusion chemotherapy (HAIC), which utilize tumor hypervascularity and allow for selective delivery of
chemotherapeutic agents to the tumor. TACE is conventionally performed by injection of an oil emulsion of
a chemotherapeutic drug, such as cisplatin or doxorubicin, followed by embolization. Alternatively, it can
be performed by delivery of embolic drug-eluting beads (DEB). Historically, the survival benefit of TACE
yielded contradictory survival benefits due to the heterogeneous selection of patients for treatment. A meta-
analysis showed an improved 2-year survival of unresectable HCC receiving arterial embolization or
chemoembolization compared to conservative treatment . On the contrary, another meta-analysis
[16]
reported no significant increase in overall survival in patients treated with TACE vs. placebo, sham, or no
[6]
intervention . TACE seems to offer a tolerable safety profile with low adverse events-related mortality.
However, increased TACE sessions lead to an increased risk of hepatic injury .
[17]
A relatively more recent method is selective internal radiation therapy (SIRT) or trans-arterial
radioembolization (TARE). Instead of causing ischemia to the tumor, TARE delivers smaller particles to
deliver radiation to the tumor, most popularly Y b-emitting isotope. Radioembolization is advantageous
90
due to lower toxicity and being an option in patients with portal vein thrombus. A comparative analysis