Page 88 - Read Online
P. 88
Page 6 of 9 Malerba et al. Hepatoma Res 2021;7:19 I http://dx.doi.org/10.20517/2394-5079.2020.131
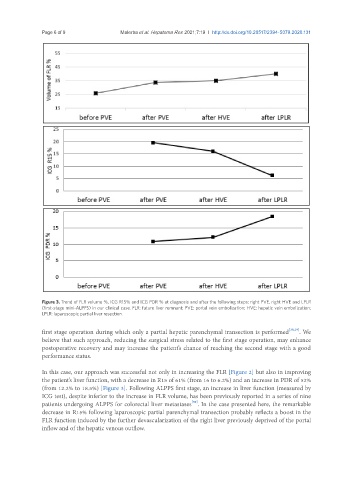
Figure 3. Trend of FLR volume %, ICG R15% and ICG PDR % at diagnosis and after the following steps: right PVE, right HVE and LPLR
(first-stage mini-ALPPS) in our clinical case. FLR: future liver remnant; PVE: portal vein embolization; HVE: hepatic vein embolization;
LPLR: laparoscopic partial liver resection.
first stage operation during which only a partial hepatic parenchymal transection is performed [28,29] . We
believe that such approach, reducing the surgical stress related to the first stage operation, may enhance
postoperative recovery and may increase the patient’s chance of reaching the second stage with a good
performance status.
In this case, our approach was successful not only in increasing the FLR [Figure 2] but also in improving
the patient’s liver function, with a decrease in R15 of 61% (from 16 to 6.2%) and an increase in PDR of 52%
(from 12.2% to 18.5%) [Figure 3]. Following ALPPS first stage, an increase in liver function (measured by
ICG test), despite inferior to the increase in FLR volume, has been previously reported in a series of nine
[30]
patients undergoing ALPPS for colorectal liver metastases . In the case presented here, the remarkable
decrease in R15% following laparoscopic partial parenchymal transection probably reflects a boost in the
FLR function induced by the further devascularization of the right liver previously deprived of the portal
inflow and of the hepatic venous outflow.