Page 43 - Read Online
P. 43
Page 6 of 14 Russo et al. Hepatoma Res 2018;4:25 I http://dx.doi.org/10.20517/2394-5079.2018.52
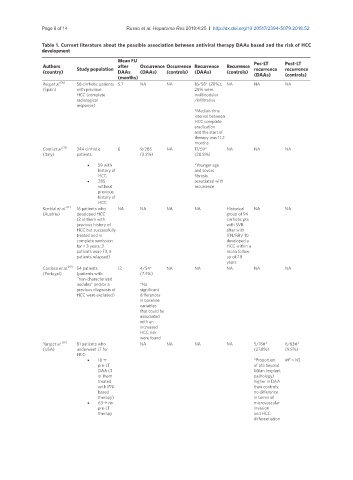
Table 1. Current literature about the possible association between antiviral therapy DAAs based and the risk of HCC
development
Mean FU
Authors Study population after Occurrence Occurrence Recurrence Recurrence Pos-LT Post-LT
recurrence
recurrence
(country) DAAs (DAAs) (controls) (DAAs) (controls)
(months) (DAAs) (controls)
Reig et al. [10] 58 cirrhotic patients 5.7 NA NA 16/58* (28%); NA NA NA
(Spain) with previous 25% were
HCC (complete multinodular
radiological /infiltrative
response)
*Median time
interval between
HCC complete
eradication
and the start of
therapy was 11.2
months
Conti et al. 344 cirrhotic 6 9/285 NA 17/59* NA NA NA
[11]
(Italy) patients: (3.2%) (28.8%)
• 59 with *Younger age
history of and severe
HCC fibrosis
• 285 associated with
without recurrence
previous
history of
HCC
[12]
Kozbial et al. 16 patients who NA NA NA NA Historical NA NA
(Austria) developed HCC group of 94
(3 of them with cirrhotic pts
previous history of with SVR
HCC but successfully after with
treated and in IFN/RBV 10
complete remission developed a
for > 3 years; 3 HCC within a
patients were F3, 5 mean follow-
patients relapsed) up of 7.8
years
Cardoso et al. [19] 54 patients 12 4/54* NA NA NA NA NA
(Portugal) (patients with (7.4%)
‘‘non-characterized
nodules” and/or a *No
previous diagnosis of significant
HCC were excluded) differences
in baseline
variables
that could be
associated
with an
increased
HCC risk
were found
Yang et al. [38] 81 patients who NA NA NA NA 5/18#* 6/63#*
(USA) underwent LT for (27.8%) (9.5%)
HCC:
• 18 > *Proportion #P = NS
pre-LT of pta beyond
DAA (3 Milan (explant
of them pathology)
treated higher in DAA
with IFN than controls;
based no difference
therapy) in terms of
• 63 > no microvascular
pre-LT invasion
therapy and HCC
differentiation