Page 105 - Read Online
P. 105
Page 8 of 23 Thonglert et al. Hepatoma Res 2023;9:40 https://dx.doi.org/10.20517/2394-5079.2023.47
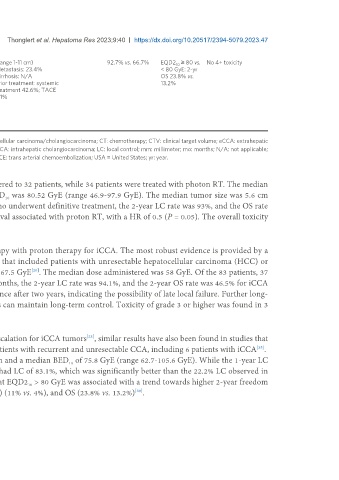
- CTV = ITV (range 1-11 cm) 92.7% vs. 66.7% EQD2 ≥ 80 vs. No 4+ toxicity
10
- PTV = ITV + (5-7) mm Metastasis: 23.4% < 80 GyE: 2-yr
Dose Cirrhosis: N/A OS 23.8% vs.
> 2cm from GI organs: 66- Prior treatment: systemic 13.2%
80 Gy in 10 F; < 2 cm from treatment 42.6%; TACE
GI organs: 45-60 Gy in 10 2.1%
F; median EQD2 80.0 GyE
(54.4-120)
Technique: double-
scattering
+
*results only iCCA or cHCC/CCA patients; results only curative subgroup; cHCC/CCA: combined hepatocellular carcinoma/cholangiocarcinoma; CT: chemotherapy; CTV: clinical target volume; eCCA: extrahepatic
cholangiocarcinoma; F: fractions; G: grade; GTV: gross tumor volume; GB: gallbladder cancer; Gy: gray; iCCA: intrahepatic cholangiocarcinoma; LC: local control; mm: millimeter; mo: months; N/A: not applicable;
NO. number: OS: overall survival; PS: passive scattering; PTV: planning target volume; RT: radiotherapy; TACE: trans arterial chemoembolization; USA = United States; yr: year.
unresectable iCCA treated with hypofractionated RT. Proton RT was administered to 32 patients, while 34 patients were treated with photon RT. The median
dose was 58.05 Gy (range 37.5-67.5 GyE) in 15 fractions, and the median BED was 80.52 GyE (range 46.9-97.9 GyE). The median tumor size was 5.6 cm
10
(range 2.5-16 cm). The median follow-up was 14 months. Of the 51 patients who underwent definitive treatment, the 2-year LC rate was 93%, and the OS rate
was 62%. A multivariate analysis of OS revealed a tendency for improved survival associated with proton RT, with a HR of 0.5 (P = 0.05). The overall toxicity
rate of grade 3 or higher was 11%, and one patient experienced RILD .
[22]
To date, no phase III randomized controlled trial has compared photon therapy with proton therapy for iCCA. The most robust evidence is provided by a
single-arm, phase II multi-institutional study conducted in the United States that included patients with unresectable hepatocellular carcinoma (HCC) or
iCCA who underwent 15 fractions of PBT, receiving a maximum total dose of 67.5 GyE . The median dose administered was 58 GyE. Of the 83 patients, 37
[20]
had iCCA, and 2 had a mix of HCC/iCCA. With a median follow-up of 19.5 months, the 2-year LC rate was 94.1%, and the 2-year OS rate was 46.5% for iCCA
patients. In particular, four additional patients with iCCA experienced recurrence after two years, indicating the possibility of late local failure. Further long-
term follow-up is required to determine whether these hypofractionated doses can maintain long-term control. Toxicity of grade 3 or higher was found in 3
patients (7.7%).
Similar to photon-based studies showing potential benefits for radiation dose escalation for iCCA tumors , similar results have also been found in studies that
[23]
have employed PBT for iCCA. The Makita et al. study used PBT to treat 28 patients with recurrent and unresectable CCA, including 6 patients with iCCA .
[35]
The median dose was 62.8 GyE (range 50.6-80 GyE) with 2-3.2 GyE per fraction and a median BED of 75.8 GyE (range 62.7-105.6 GyE). While the 1-year LC
10
rate was 67.7% (95% CI: 56.3%-79.1%), patients who received BED > 70 GyE had LC of 83.1%, which was significantly better than the 22.2% LC observed in
10
those with BED < 70 GyE (P = 0.002). The study by Kim et al. also showed that EQD2 > 80 GyE was associated with a trend towards higher 2-year freedom
10
10
from local progression (FFLP) (92.7% vs. 66.7%), progression-free survival (PFS) (11% vs. 4%), and OS (23.8% vs. 13.2%) .
[39]