Page 12 - Read Online
P. 12
Page 614 Laubach et al. Cancer Drug Resist 2023;6:611-41 https://dx.doi.org/10.20517/cdr.2023.60
+
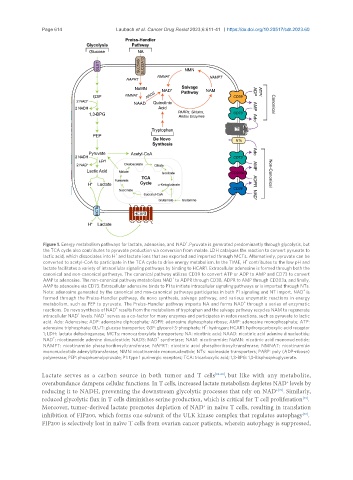
Figure 1. Energy metabolism pathways for lactate, adenosine, and NAD . Pyruvate is generated predominantly through glycolysis, but
the TCA cycle also contributes to pyruvate production via conversion from malate. LDH catalyzes the reaction to convert pyruvate to
+
lactic acid, which dissociates into H and lactate ions that are exported and imported through MCTs. Alternatively, pyruvate can be
+
converted to acetyl-CoA to participate in the TCA cycle to drive energy metabolism. In the TIME, H contributes to the low pH and
lactate facilitates a variety of intracellular signaling pathways by binding to HCAR1. Extracellular adenosine is formed through both the
canonical and non-canonical pathways. The canonical pathway utilizes CD39 to convert ATP or ADP to AMP and CD73 to convert
+
AMP to adenosine. The non-canonical pathway metabolizes NAD to ADPR through CD38, ADPR to AMP through CD203a, and finally,
AMP to adenosine via CD73. Extracellular adenosine binds to P1 to initiate intracellular signaling pathways or is imported through NTs.
+
Note: adenosine generated by the canonical and non-canonical pathways participates in both P1 signaling and NT import. NAD is
formed through the Preiss-Handler pathway, de novo synthesis, salvage pathway, and various enzymatic reactions in energy
+
metabolism, such as PEP to pyruvate. The Preiss-Handler pathway imports NA and forms NAD through a series of enzymatic
+
reactions. Do novo synthesis of NAD results from the metabolism of tryptophan and the salvage pathway recycles NAM to regenerate
+
+
intracellular NAD levels. NAD serves as a co-factor for many enzymes and participates in redox reactions, such as pyruvate to lactic
acid. Ado: Adenosine; ADP: adenosine diphosphate; ADPR: adenosine diphosphate ribose; AMP: adenosine monophosphate; ATP:
+
adenosine triphosphate; GLUT: glucose transporter; G3P: glycerol-3-phosphate; H : hydrogen; HCAR1: hydroxycarboxylic acid receptor
1; LDH: lactate dehydrogenase; MCTs: monocarboxylate transporters; NA: nicotinic acid; NAAD: nicotinic acid adenine dinucleotide;
+ +
NAD : nicotinamide adenine dinucleotide; NADS: NAD synthetase; NAM: nicotinamide; NaMN: nicotinic acid mononucleotide;
NAMPT: nicotinamide phosphoribosyltransferase; NAPRT: nicotinic acid phosphoribosyltransferase; NMNAT: nicotinamide
mononucleotide adenylyltransferase; NMN: nicotinamide mononucleotide; NTs: nucleoside transporters; PARP: poly (ADP-ribose)
polymerase; PEP: phosphoenolpyruvate; P1: type 1 purinergic receptors; TCA: tricarboxylic acid; 1,3-BPG: 1,3-Bisphosphoglycerate.
Lactate serves as a carbon source in both tumor and T cells [26-28] , but like with any metabolite,
+
overabundance dampens cellular functions. In T cells, increased lactate metabolism depletes NAD levels by
reducing it to NADH, preventing the downstream glycolytic processes that rely on NAD . Similarly,
+[29]
[29]
reduced glycolytic flux in T cells diminishes serine production, which is critical for T cell proliferation .
Moreover, tumor-derived lactate promotes depletion of NAD in naïve T cells, resulting in translation
+
inhibition of FIP200, which forms one subunit of the ULK kinase complex that regulates autophagy .
[30]
FIP200 is selectively lost in naïve T cells from ovarian cancer patients, wherein autophagy is suppressed,