Page 220 - Read Online
P. 220
Sahulee et al. Vessel Plus 2022;6:5 https://dx.doi.org/10.20517/2574-1209.2021.94 Page 3 of 10
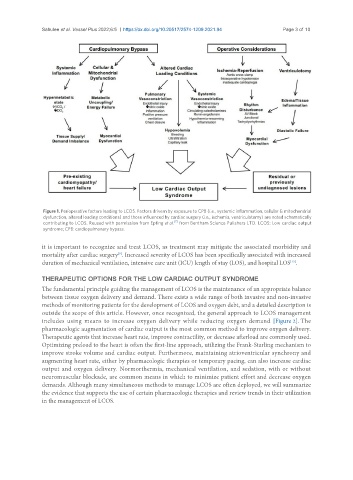
Figure 1. Perioperative factors leading to LCOS. Factors drivern by exposure to CPB (i.e., systemic inflammation, cellular & mitochondrial
dysfunction, altered loading conditions) and those influenced by cardiac surgery (i.e., ischemia, ventriculotomy) are noted schematically
[7]
contributing to LCOS. Reused with permission from Epting et al. from Bentham Science Pulishers LTD. LCOS: Low cardiac output
syndrome; CPB: cardiopulmonary bypass.
it is important to recognize and treat LCOS, as treatment may mitigate the associated morbidity and
mortality after cardiac surgery . Increased severity of LCOS has been specifically associated with increased
[9]
duration of mechanical ventilation, intensive care unit (ICU) length of stay (LOS), and hospital LOS .
[13]
THERAPEUTIC OPTIONS FOR THE LOW CARDIAC OUTPUT SYNDROME
The fundamental principle guiding the management of LCOS is the maintenance of an appropriate balance
between tissue oxygen delivery and demand. There exists a wide range of both invasive and non-invasive
methods of monitoring patients for the development of LCOS and oxygen debt, and a detailed description is
outside the scope of this article. However, once recognized, the general approach to LCOS management
includes using means to increase oxygen delivery while reducing oxygen demand [Figure 2]. The
pharmacologic augmentation of cardiac output is the most common method to improve oxygen delivery.
Therapeutic agents that increase heart rate, improve contractility, or decrease afterload are commonly used.
Optimizing preload to the heart is often the first-line approach, utilizing the Frank-Starling mechanism to
improve stroke volume and cardiac output. Furthermore, maintaining atrioventricular synchrony and
augmenting heart rate, either by pharmacologic therapies or temporary pacing, can also increase cardiac
output and oxygen delivery. Normorthermia, mechanical ventilation, and sedation, with or without
neuromuscular blockade, are common means in which to minimize patient effort and decrease oxygen
demands. Although many simultaneous methods to manage LCOS are often deployed, we will summarize
the evidence that supports the use of certain pharmacologic therapies and review trends in their utilization
in the management of LCOS.