Page 873 - Read Online
P. 873
Farber et al. Plast Aesthet Res 2020;7:72 I http://dx.doi.org/10.20517/2347-9264.2020.152 Page 23 of 28
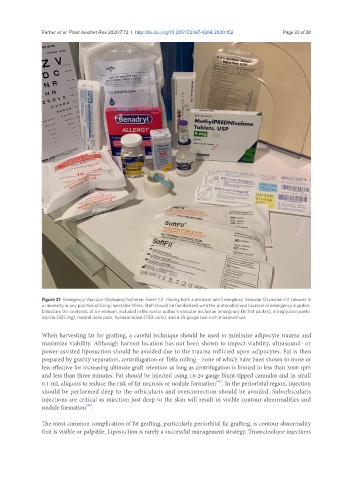
Figure 21. Emergency Vascular Occlusion/Ischemic Event Kit. Having both a protocol and Emergency Vascular Occlusion Kit (above) is
a necessity in any practice utilizing injectable fillers. Staff should be familiarized with the protocol(s) and location of emergency supplies.
Listed are the contents, at a minimum, included in the senior author’s vascular occlusion emergency kit: hot pack(s), nitroglycerin paste.
aspirin (325 mg), medrol dose pack, hyaluronidase (750 units), and a 25-gauge two-inch microcannula
When harvesting fat for grafting, a careful technique should be used to minimize adipocyte trauma and
maximize viability. Although harvest location has not been shown to impact viability, ultrasound- or
power-assisted liposuction should be avoided due to the trauma inflicted upon adipocytes. Fat is then
prepared by gravity separation, centrifugation or Telfa rolling - none of which have been shown to more or
less effective for increasing ultimate graft retention as long as centrifugation is limited to less than 3000 rpm
and less than three minutes. Fat should be injected using 18-20 gauge blunt-tipped cannulas and in small
[51]
0.1 mL aliquots to reduce the risk of fat necrosis or nodule formation . In the periorbital region, injection
should be performed deep to the orbicularis and overcorrection should be avoided. Suborbicularis
injections are critical as injection just deep to the skin will result in visible contour abnormalities and
[52]
nodule formation .
The most common complication of fat grafting, particularly periorbital fat grafting, is contour abnormality
that is visible or palpable. Liposuction is rarely a successful management strategy. Triamcinolone injections